It was not until I started struggling with both weight gain and rising blood pressure that I truly began to connect the dots between the two.
Like many people, I had heard that carrying extra pounds could affect my heart health, but I was not entirely sure how.
Then, after a few doctor visits and some scary readings from my blood pressure monitor, it became clear: obesity and high blood pressure are closely linked.
But how exactly does obesity raise your blood pressure levels?
In this article, leanandfit.info shall dive deep into the science behind how excess weight puts stress on your cardiovascular system and what it does to your blood pressure.
We would explore the mechanisms that connect obesity to hypertension, real-life examples from daily life, and the relationship between Body Mass Index (BMI) and blood pressure.
By the end of this article, you would have a clearer understanding of why obesity and hypertension often go hand in hand.
In This Article:
- What is Blood Pressure, and Why Does It Matter?
- The Connection Between Obesity and High Blood Pressure
- How Excess Fat Contributes to Hypertension
- The Role of Visceral Fat in Blood Pressure Elevation
- Understanding the BMI and Blood Pressure Relationship
- How Obesity Affects Heart and Blood Vessel Function
- Real-Life Examples: Obesity and Blood Pressure in Daily Life
- FAQs on Blood Pressure and Weight Loss
- The Compounding Effects of Obesity on Hypertension
- Conclusion: How and Why Obesity Increases Blood Pressure
What is Blood Pressure, and Why Does It Matter?
Before we dive into the connection between obesity and blood pressure, let us first understand what blood pressure actually is.
Blood pressure is the force of your blood pushing against the walls of your arteries as your heart pumps blood through your body.
When blood pressure is too high, it puts extra strain on your heart and blood vessels, leading to an increased risk of heart disease, gut dysbiosis, stroke, and kidney issues.
For those of us carrying extra weight, this becomes particularly important because the heart has to work harder to pump blood through a larger body, which can increase blood pressure.
The Connection Between Obesity and High Blood Pressure
Obesity and high blood pressure (hypertension) are often mentioned together, and for good reason.
Studies show that people with obesity are at a significantly higher risk of developing hypertension compared to those with a healthy weight.
In fact, obesity is one of the leading risk factors for high blood pressure worldwide.
But why is that?
I wondered the same thing when my doctor first pointed out that my rising weight might be contributing to my elevated blood pressure.
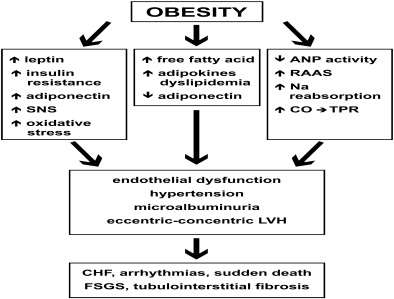
As it turns out, there are several mechanisms at play, and it is not just about the physical weight.
Research published in the Journal of Hypertension demonstrates that obesity affects the balance of hormones, the function of blood vessels, and even how the kidneys manage salt.
This combination of factors creates a perfect storm for high blood pressure in obesity.
How Excess Fat Contributes to Hypertension?
When you carry extra weight, especially fat, it does more than add inches to your waistline.
As per leanandfit.info, “Fat tissue is metabolically active, meaning it does not just sit there—it releases hormones and substances that can interfere with blood pressure regulation”.
For example, excess fat increases the production of leptin, a hormone that controls appetite but also affects the sympathetic nervous system, which can raise blood pressure.
Additionally, fat cells produce cytokines—proteins that cause inflammation in the body. This inflammation can lead to stiffening of the arteries, making it harder for blood to flow smoothly, resulting in elevated blood pressure.
I noticed these effects firsthand.
After gaining a significant amount of weight, I started feeling more fatigued, and my blood pressure readings spiked.
It was not just the extra pounds themselves but how my body responded to that weight gain.
The Role of Visceral Fat in Blood Pressure Elevation
Not all fat is created equal, and one type of fat—visceral fat—is particularly harmful when it comes to blood pressure.
Visceral fat is the fat stored around your internal organs, deep inside your abdomen.
This type of fat is much more dangerous than the subcutaneous fat that sits just under the skin.
Visceral fat releases more inflammatory substances and hormones that lead to hypertension.
It also pushes against your internal organs, including the kidneys, which play a crucial role in regulating blood pressure.
The more visceral fat you carry, the higher the risk of developing hypertension in obesity.
In my own life, I found that reducing belly fat helped improve my blood pressure readings, which confirmed just how significant visceral fat can be for cardiovascular health.
Understanding the BMI and Blood Pressure Relationship
Body Mass Index (BMI) is a tool often used to measure whether a person has a healthy weight for their height.
A higher BMI typically indicates overweight or obesity, which, as we have discussed, can increase the risk of hypertension.
The relationship between BMI and blood pressure is well-established. According to research from the National Heart, Lung, and Blood Institute, as BMI increases, so does the likelihood of high blood pressure.
This is because higher BMI often indicates more body fat, which puts strain on the heart and blood vessels.
For me, this was an eye-opener. My BMI had slowly crept up over the years, and alongside it, my blood pressure readings followed.
Even losing a small amount of weight made a noticeable difference in my blood pressure, proving that the BMI and hypertension connection is a real and measurable phenomenon.
How Obesity Affects Heart and Blood Vessel Function?
Carrying excess weight affects how the heart and blood vessels function.
When you are overweight, your heart has to pump harder to circulate blood throughout your body.
This increased workload can cause the heart muscle to thicken, a condition known as left ventricular hypertrophy, which can further increase blood pressure.
Obesity also impacts the elasticity of blood vessels.
Over time, blood vessels become stiffer due to chronic inflammation and the increased workload, which makes it harder for blood to flow freely. This leads to higher pressure within the arteries, known as hypertension.
In my daily life, I noticed these changes through physical symptoms.
Activities that were once easy, like climbing stairs, became more challenging as my heart struggled to keep up. My blood pressure readings confirmed the strain my cardiovascular system was under.
FAQs on Blood Pressure and Weight Loss
Q-1: How does belly fat make the kidneys “choose” higher blood pressure?
A-1: Central adiposity increases pressure around the kidneys and loads them with fatty infiltration. That physical squeeze plus local inflammation makes the kidneys retain more sodium and water. At the same time, the renin–angiotensin–aldosterone system (RAAS) gets chronically nudged on, so blood vessels constrict and fluid volume rises. The combo—tighter vessels + more volume—sets a higher pressure “set point.” Practical lever: reduce sodium and raise potassium (produce, legumes, dairy) while losing even 5–10% body weight; this lowers intrarenal pressure and deactivates RAAS over weeks.
Q-2: Which fat-derived signals push nerves and hormones to keep pressure high?
A-2: Enlarged fat tissue doesn’t just store energy—it signals. Higher leptin and insulin levels stimulate the sympathetic nervous system, especially to the kidneys and blood vessels, increasing heart rate, vascular tone, and sodium reabsorption. Many people with obesity also show aldosterone excess out of proportion to RAAS, which further drives salt/water retention. Practical lever: prioritize sleep regularity and a protein-plus-fiber meal pattern to improve leptin/insulin sensitivity; add two to three weekly resistance sessions to dial down sympathetic drive at rest.
Q-3: Why does sleep apnea in obesity send nighttime blood pressure through the roof?
A-3: Repeated airway collapse triggers oxygen dips and abrupt arousals. Each event jolts the sympathetic system, spikes blood pressure, and stiffens vessels; over months, the body loses its normal “nighttime dip,” a pattern linked to higher cardiovascular risk. Treating sleep apnea (weight loss, side-sleeping, oral devices, or CPAP when indicated) often improves morning headaches, lowers resting heart rate, and restores a healthier nocturnal profile—benefits you can amplify with evening alcohol/salt limits and a consistent wind-down routine.
Q-4: Why does weight gain make me salt-sensitive—and how can I test this safely at home?
A-4: In obesity, kidneys become less efficient at excreting sodium, vascular smooth muscle is primed to constrict, and endothelial nitric oxide (a vessel relaxer) runs low.
The result: a salty meal raises pressure more and for longer than it would at a lower weight. A simple two-week self-audit: keep steps, meds, and fluids steady; monitor blood pressure morning/evening; alternate 3–4 days of higher-salt eating with 3–4 days of lower-salt, higher-potassium meals.
If averages drop ≥5–7 mmHg on lower-salt days, you’re salt-sensitive—great news, because you can harvest quick wins by cooking more at home, choosing unsalted staples, and loading plates with potassium-rich plants while you work on gradual weight reduction.
Real-Life Examples: Obesity and Blood Pressure in Daily Life
Obesity’s impact on blood pressure is not just a theory—it is something that many of us experience in daily life.
Simple tasks like walking long distances or lifting heavy objects became much more difficult as my weight increased. These tasks caused my heart to race and my blood pressure to spike.
Similarly, lifestyle factors like consuming added sugar in fast food, lack of physical inactivity, and even stress can exacerbate the problem. A high-sodium diet, for example, is common in individuals with obesity and leads to fluid retention, which raises blood pressure.
Sedentary habits only compound the issue, as physical inactivity contributes to both weight gain and hypertension.
I had to make conscious changes to my daily routine (doing push-ups to develop my upper body strength) to see improvements in both my weight and blood pressure.
These lifestyle modifications didn’t happen overnight, but they were necessary steps in controlling both conditions.
The Compounding Effects of Obesity on Hypertension
Let’s be blunt: obesity and high blood pressure are like the worst kind of roommates—they feed off each other’s bad habits and wreck the place (in this case, your cardiovascular system).
Obesity does not just trigger hypertension—it practically fuels it with rocket-grade intensity. Excess fat, especially around the abdomen, increases blood volume and cardiac output. This means your heart has to pump harder to circulate blood, raising your blood pressure like a geyser under pressure.
Worse still, fat tissue releases hormones and inflammatory substances that stiffen arteries and disrupt the balance of sodium and water—classic triggers for hypertension.
Now throw insulin resistance into the mix. As body weight increases owing to sedentary behavior, your cells stop responding properly to insulin.
This not only sets the stage for type 2 diabetes but also worsens blood pressure control. One study found that nearly 70% of people with diabetes also have high blood pressure—talk about a toxic duo.
And it does not stop there. Obesity-related hypertension is a gateway drug to even bigger problems—stroke, heart disease, and kidney failure.
Your kidneys, those underappreciated filtration units, struggle under increased pressure and excess fat. That’s why hypertension in obese individuals is a leading cause of chronic kidney disease.
Real-life example?
A patient named Ravi (let’s call him that) weighed 270 pounds and had a blood pressure reading of 165/105. His doctor warned that each extra 10 pounds was pushing his heart closer to the danger zone.
After losing just 25 pounds through a combination of brisk walking and a low-sodium diet, his BP dropped by nearly 15 points. Proof that small shifts can lead to major changes.
Ultimately, managing obesity and hypertension is not about choosing one battle—it is about fighting the entire war. Because in the world of metabolic health, these conditions do not live in isolation.
They multiply their damage like compound interest on a bad credit card. The sooner you intervene, the better your chances of staying ahead of the avalanche.

Takeaway: How Obesity Increases Your Blood Pressure Levels?
So, how does obesity increase your blood pressure levels?
The answer lies in the complex interaction between excess body fat, chronic inflammation, hormonal imbalances, and cardiovascular strain.
Obesity puts extra pressure on the heart and blood vessels, leading to hypertension in many individuals.
Whether through the accumulation of visceral fat, changes in hormone production, or simple mechanical strain, obesity creates a perfect environment for elevated blood pressure.
The relationship between BMI and blood pressure makes it clear: as weight increases, so does the risk of hypertension.
In my experience, the link between obesity and high blood pressure was undeniable.
By understanding the mechanisms behind it, I was better equipped to manage both my weight and my blood pressure.
While there is no one-size-fits-all solution, recognizing this connection can be a powerful first step toward better health.
References: