Let’s be honest—our modern world does not make it easy to stay fit.
With fast food on every corner and so much time spent in front of screens, it is no surprise that obesity has become a global epidemic.
But did you know that obesity is more than just a weight issue?
It is deeply connected to hormonal imbalances that can lead to depression.
In this article, we will explore how obesity affects our hormones and why this often results in depressive symptoms.
In This Article:
- Introduction to the Obesity-Depression Connection
- The Hormonal Imbalances Associated with Obesity
- How These Imbalances Affect Mood
- Real-Life Impacts: The Vicious Cycle of Obesity and Depression
- Breaking the Cycle: Treatment Options and Lifestyle Changes
- Conclusion: Managing Hormones and Mental Health
Introduction to the Obesity-Depression Connection
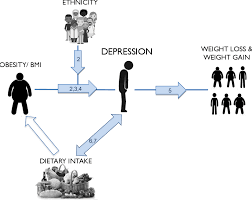
Obesity and depression are intricately linked, each influencing the onset and progression of the other.
This bidirectional relationship is supported by substantial research indicating that individuals with obesity are at a higher risk of developing depression, and those with depression have an increased likelihood of becoming obese.
A study published in the Journal of Psychiatry and Neuroscience highlights that obesity elevates the risk of depression by 55%, while depression increases the risk of obesity by 58%.
This interconnectedness can be attributed to various factors, including hormonal imbalances, social stigmatization, and lifestyle behaviors.
Hormonal Influences:
Adipose tissue, commonly known as body fat, functions as an endocrine organ by secreting hormones such as leptin, adiponectin, and resistin. These hormones play crucial roles in energy metabolism and appetite regulation.
For instance, leptin is an appetite suppressant, and its deficiency has been associated with severe obesity and depressive symptoms. Low plasma leptin levels are linked to depression, as leptin influences mood and cognition by inducing structural and functional changes in brain regions like the hippocampus and prefrontal cortex.
Additionally, leptin activates pathways associated with dopamine and mTOR, enhancing synaptogenesis, which is vital for neuroplasticity (Source: Wikipedia, Adipose-derived hormones).
Furthermore, estrogen, a hormone predominantly found in women, plays a significant role in mental health. Fluctuating or low estrogen levels have been correlated with mood disturbances.
Clinical recovery from postpartum, perimenopausal, and postmenopausal depression has been effective after stabilizing or restoring estrogen levels.
This suggests that hormonal changes, such as those occurring during menopause, can influence both mood regulation and weight, potentially linking obesity and depression (Source: Wikipedia, Estrogen).
Social Stigmatization and Mental Health:
Individuals with obesity often face societal stigma and discrimination, leading to psychological distress. This stigmatization is associated with increased risks of depression, anxiety, and lowered self-esteem.
Experiencing weight stigma can result in maladaptive eating patterns, such as binge eating, decreased motivation for physical activity, and avoidance of healthcare services, thereby perpetuating both obesity and depression (Source: Wikipedia, Social stigma of obesity).
Lifestyle Factors:
Depression can lead to behaviors that contribute to weight gain, including decreased physical activity and increased consumption of high-calorie foods.
Conversely, obesity can lead to depression through mechanisms such as social isolation and reduced mobility.
Understanding this bidirectional relationship is crucial for developing effective interventions that address both conditions simultaneously.
Childhood and Adolescence:
The relationship between obesity and depression is also evident in younger populations. Obese children often experience bullying and social marginalization, leading to low self-esteem and depression.
These psychological issues can persist into adulthood, increasing the risk of chronic health conditions.
Addressing obesity and mental health early in life is essential to prevent long-term adverse outcomes (Source: Wikipedia, Psychological aspects of childhood obesity).
Important Tip:
The complex interplay between obesity and depression involves hormonal, psychological, and behavioral factors.
Recognizing this bidirectional relationship is vital for healthcare providers to develop comprehensive treatment plans that address both physical and mental health aspects, ultimately improving patient outcomes.
The Hormonal Imbalances Associated with Obesity
Obesity is not merely about carrying extra weight; it profoundly impacts the body’s hormonal systems.
When fat accumulates, particularly around the abdomen, it is not just sitting there passively.
Fat tissue is biologically active and produces hormones and inflammatory molecules, which can disrupt the body’s natural hormone balance.
This is where things start to get tricky:
- Cortisol, the Stress Hormone: Individuals who are overweight often have elevated cortisol levels due to chronic stress.
This hormone, while essential in small amounts, can become problematic when it remains elevated, leading to a constant state of stress.
This prolonged stress state increases the risk of depression (Healthline, 2023).
- Insulin Resistance: Obesity is a major contributor to insulin resistance, a condition where the body doesn’t respond properly to insulin.
This results in elevated blood sugar levels, which can also disrupt mood regulation.
A study published in Diabetes Care highlighted how insulin resistance not only predisposes individuals to diabetes but also affects brain function, increasing depression risk (Harvard Health, 2023).
- Leptin and Ghrelin, the Hunger Hormones: Leptin and ghrelin regulate hunger and satiety.
In obese individuals, leptin resistance often develops, meaning the brain does not receive the signal that the body is full.
This imbalance contributes to overeating and further weight gain, while also playing a role in mood swings and depressive symptoms (CentreSpring MD, 2023).
How These Imbalances Affect Mood?
Now, let’s connect the dots.
When hormones like cortisol and insulin are out of balance, they create a cascade of effects on the body’s systems:
Inflammation:
Obesity increases inflammation in the body, which has been directly linked to depression. Inflammation affects neurotransmitter production, including serotonin, which is responsible for regulating mood.
According to a study published in Nature Reviews Neuroscience, higher levels of inflammatory markers in obese individuals correlate with higher rates of depression (Springer, 2023).
Disrupted Sleep Patterns:
Hormonal imbalances in obesity also affect sleep. Poor sleep, in turn, disrupts the regulation of hunger hormones like ghrelin, contributing to increased appetite and weight gain.
Studies have shown that up to 75% of people with depression experience sleep disturbances, which are also common in those with obesity (Verywell Health, 2023). This vicious cycle makes it difficult for those who are already struggling with weight and mood to find relief.
Thyroid Hormone Dysfunction:
Thyroid hormones play a significant role in metabolism and mood. Obesity is often linked to hypothyroidism, where the thyroid gland does not produce enough hormones, leading to weight gain and mood disturbances.
This connection highlights how “obesity is a hormonal imbalance” that extends beyond just diet and exercise (Medical News Today, 2023).
Real-Life Impacts: The Vicious Cycle of Obesity and Depression
Meet Amy, a 35-year-old office worker. Amy has struggled with weight since her teenage years.
With time, she noticed that her weight gain was accompanied by persistent low energy and feelings of hopelessness.
When she visited her doctor, she was diagnosed as both depressed and obese.
Her doctor explained that the high cortisol levels from her stressful job and her weight gain were both contributing to her low mood.
This story is not unique.
Many people experience a similar cycle where weight gain triggers hormonal changes that elevate the risk of depression.
Research from the Journal of Obesity and Depression indicates that excess body fat, especially visceral fat, is linked to increased production of hormones and inflammatory markers that directly influence brain function and mood regulation.

Breaking the Cycle: Treatment Options and Lifestyle Changes
Understanding the hormonal connection between obesity and depression is just the start.
To manage these conditions effectively, a multi-pronged approach is often needed:
- Diet and Nutrition: Adopting an anti-inflammatory diet can help manage both weight and mood. Diets like the Mediterranean diet have been shown to reduce depression symptoms while promoting weight loss. Incorporating foods rich in omega-3 fatty acids or drinking home made smoothies that dissolve belly fat can help balance hormones and reduce inflammation, improving mood (Healthline, 2023).
- Exercise: Regular physical activity, even something as simple as walking or yoga, can help regulate cortisol levels and boost endorphin production. Exercise is a natural way to combat both weight gain and depression, and it’s a cornerstone of many “depression and obesity treatment” programs (Verywell Health, 2023).
- Medical Interventions: In some cases, medications like metformin (for insulin resistance) or thyroid supplements may be needed to balance hormones. Consulting a healthcare professional to check for “obesity gland and effect of hormonal imbalance” is crucial, as hormone therapy may be an option for those whose weight gain is directly linked to glandular imbalances (Medical News Today, 2023).
- Therapy and Stress Management: Addressing mental health through cognitive-behavioral therapy (CBT) can help manage stress and emotional eating. Therapy has been shown to be effective in improving both weight and mood outcomes for those “depressed due to weight gain.”
Managing Hormones and Mental Health
Obesity and depression are two sides of the same coin, connected through complex hormonal pathways.
By understanding how obesity leads to hormonal imbalances and subsequently affects mood, we can take steps to manage these conditions holistically.
Whether through diet, exercise, therapy, or medical intervention, addressing both physical and mental health is key.
Breaking the cycle may not be easy, but it is possible with the right approach and support.
If you are feeling stuck or “overweight and depressed,” remember that you are not alone.
Professional help is available, and with a tailored plan that addresses both hormonal and emotional factors, you can reclaim your health and improve your quality of life.
References: