When it comes to heart health, HDL cholesterol is the golden child—often referred to as the “good cholesterol” for good reason.
It acts as a scavenger, collecting excess cholesterol from the bloodstream and transporting it back to the liver for disposal.
This process helps keep arteries clean and reduces the risk of heart disease.
But here is where the plot thickens: obesity, especially the stubborn kind that clings to your belly like a stage-five clinger, can sabotage HDL’s life-saving mission.
We are not just talking about weight on the scale—this is about visceral fat that wraps itself around internal organs and disrupts crucial metabolic functions.
Obesity does not just lower HDL levels; it also affects how HDL behaves. From increasing triglycerides to promoting chronic inflammation, excess fat throws HDL into a dysfunctional spiral.
The good guy turns less effective, losing its power to protect your arteries and combat cardiovascular disease.
This is far more serious than a lab report with slightly skewed numbers. It is a sign that your body’s cholesterol management system is breaking down.
In this article, the LeanAndFit research staff dives deep into how obesity drags HDL cholesterol down with it—and why this metabolic mess is a bigger deal than you might think.
Points Covered in this Article
- How Central Fat Silences HDL’s Party Tunes
- Adipose Tissue: The HDL Thief in the Biochemical Night
- Enzymatic Blockades: The HDL Metabolism Traffic Jam
- Inflammation, Insulin Resistance, and the HDL Domino Effect
- Altered HDL Quality: It’s Not Just the Quantity, It’s the Character
- Reverse Cholesterol Transport: When HDL Loses Driving Privileges
- FAQs on Obesity and Decreased HDL Cholesterol
- Weight Loss: The Comeback Tour for HDL
How Central Fat Silences HDL’s Party Tunes?
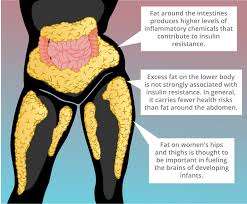
Let’s start with the obvious: belly fat is not just about squeezing into your jeans or blaming last night’s pizza.
Visceral fat—the deep, sneaky kind that hugs your organs from the inside—is far more dangerous than the stuff you can pinch.
It behaves less like passive storage and more like a hyperactive biochemical factory.
And one of its favorite pastimes? Ruining HDL cholesterol’s ability to function properly.
HDL, often dubbed the “good” cholesterol, is essential for mopping up excess cholesterol and ferrying it back to the liver.
But visceral fat throws a wrench into this life-saving routine. It floods your system with free fatty acids, cytokines and pro-inflammatory agents, which collectively impair the liver’s ability to produce and maintain healthy HDL levels.
That is like trying to throw a party while someone keeps unplugging the speakers—HDL never gets a chance to shine.
Even more mischievously, belly fat drives up triglyceride levels.
This activates a protein called CETP (cholesteryl ester transfer protein), which initiates a lipid trade that cheats HDL of its protective core. HDL ends up small, weak, and ineffective.
Think of it as losing the bouncers at a club—you still have a door, but anyone can walk in and wreck the vibe.
And here’s the kicker: even people with a “normal” BMI can have high visceral fat. Waist circumference matters more than you think.
A muffin top is not just cosmetic—it is often a silent saboteur of your HDL cholesterol.
So the next time your belt feels tight, consider it more than a wardrobe alert—it might be your body’s way of warning you about your heart health.
Adipose Tissue: The HDL Thief in the Biochemical Night
When fat cells multiply and expand, they do not just sit quietly. In obesity, adipose tissue turns into a chemically active monster that hijacks HDL particles.
Normally, HDL is built using components like cholesterol and a protein called apoA-I. But in obese individuals, fat cells hoard these raw materials, leaving less for HDL formation.
To make matters worse, the transporters responsible for moving cholesterol out of cells—ABCA1 and SR-BI—become sluggish.
So even if your body wants to make HDL, it’s working with limited ingredients and a broken conveyor belt.
The result? Less HDL is made, and what does get built is weak and ineffective.
Essentially, your fat cells are pulling off a stealthy cholesterol heist, robbing your body of the good guys.
Enzymatic Blockades: The HDL Metabolism Traffic Jam
Imagine HDL metabolism as a bustling freeway. In a lean body, traffic moves smoothly: HDL particles are formed, matured, and recycled with efficiency.
But with obesity, this freeway turns into a gridlock. One big reason is the enzyme CETP (cholesteryl ester transfer protein), which becomes overactive in obese individuals.
CETP swaps out HDL’s healthy contents for triglycerides, weakening its structure. Another culprit is hepatic lipase, which trims HDL particles down to a less functional size.
And as if that were not enough, the breakdown of apoA-I—the protein backbone of HDL—speeds up too.
All these factors shrink HDL, shorten its lifespan, and compromise its function.
It is like taking a luxury car and turning it into a rusty hatchback: it still moves, but not impressively.
Inflammation, Insulin Resistance, and the HDL Domino Effect
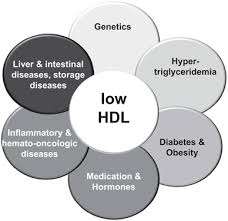
Obesity is not just about extra calories—it is about chronic and low-grade inflammation. Fat tissue in obese individuals releases pro-inflammatory cytokines like TNF-alpha and IL-6.
These inflammatory agents do not just cause aches and pains; they mess with cholesterol transporters, reducing HDL formation.
At the same time, this inflammation promotes insulin resistance, a condition where cells ignore insulin’s call. As insulin resistance builds, free fatty acids flood the bloodstream, pushing the liver to pump out more VLDL particles—fat carriers that compete with HDL.
VLDL essentially bullies HDL out of the spotlight, taking up enzymes and particles that HDL needs to survive.
The net result?
A downward spiral where inflammation and jeopardized glucose metabolism tag-team HDL into oblivion. It is a biochemical domino effect, and HDL is the last one standing—and falling.
Altered HDL Quality: It is Not Just the Quantity, It is the Character
If you think of HDL as the “good guy,” obesity doesn’t just reduce his numbers—it corrupts his personality.
In lean individuals, HDL particles are large, buoyant, and packed with antioxidant and anti-inflammatory power. But in people with obesity, HDL becomes small, dense, and dysfunctional.
It is still technically HDL, but it cannot do its job properly. These altered particles are poor at picking up cholesterol and are less protective for blood vessels.
Even worse, they can become pro-inflammatory under stress—meaning they may join the dark side.
So when doctors measure HDL cholesterol in obese patients, the number might look okay, but the particles themselves may be metabolically broken.
This proves once again: quality matters just as much—if not more—than quantity.
Reverse Cholesterol Transport: When HDL Loses Driving Privileges?
One of HDL’s most important roles is reverse cholesterol transport—essentially shuttling excess cholesterol from the arteries back to the liver for disposal.
In a healthy system, this is a smooth ride. But with obesity, the engine sputters. Cholesterol transporters like ABCA1 and ABCG1 become less active due to inflammation and insulin resistance. As a result, HDL can’t gather cholesterol efficiently.
Add in the excessive CETP activity, and whatever cholesterol HDL does collect often ends up being redirected to LDL and VLDL instead of the liver.
This is the molecular equivalent of HDL losing its driver’s license. The cholesterol builds up in arteries, increasing the risk of cardiovascular diseases such as high blood pressure.
So even if HDL is present, its ability to do its job—clear the roads of cholesterol traffic—is seriously compromised.
FAQs on Obesity and Decreased HDL Cholesterol
Q-1: How does obesity lead to decreased HDL cholesterol levels?
A-1: Obesity, especially excess fat around the abdomen, causes an increase in harmful cholesterol particles and disrupts the balance of lipids in the body. This imbalance often results in lowered levels of HDL cholesterol, which is crucial for removing bad cholesterol from the bloodstream.
Q-2: What role does adipose tissue play in the relationship between obesity and HDL cholesterol?
A-2: Fat tissue, particularly the fat stored around internal organs, releases substances that promote inflammation and interfere with the normal metabolism of HDL cholesterol. This disruption decreases HDL levels and alters its protective functions, increasing cardiovascular risk.
Q-3: Are there specific HDL subfractions affected by obesity?
A-3: Yes, obesity tends to reduce the larger, more protective HDL particles while increasing smaller, less effective HDL particles. The smaller HDL particles are not as efficient at removing cholesterol from the arteries, which diminishes HDL’s cardiovascular benefits.
Q-4: How does weight loss impact HDL cholesterol levels in obese individuals?
A-4: Losing weight can improve HDL cholesterol levels significantly. Even moderate weight loss helps restore healthier lipid profiles by increasing HDL cholesterol and lowering triglycerides, reducing the risk of heart disease.
Q-5: Can dietary changes influence HDL cholesterol levels in the context of obesity?
A-5: Yes, changes in diet can improve HDL cholesterol levels in obese individuals. Consuming more healthy fats, such as those found in nuts, seeds, and fish, while minimizing harmful trans fats, can raise HDL levels and support cardiovascular health.
Weight Loss: The Comeback Tour for HDL
Now for some good news—HDL loves a comeback story. Studies consistently show that losing even a small percentage of body weight (around 5–10%) can significantly raise HDL levels.
This is especially true when the weight loss comes from reducing visceral fat.
Exercise—particularly aerobic workouts—boosts the enzymes that support HDL production and function. Dietary changes help too, especially diets rich in monounsaturated fats like olive oil, nuts, and fatty fish.
Bariatric surgery has also been shown to restore HDL levels and improve particle quality.
The key takeaway?
HDL is resilient. Give it a better environment—less fat, fewer inflammatory signals, more physical movement—and it will rise again.
And this time, it comes back stronger, larger, and more functional, ready to reclaim its title as heart health’s MVP.
Bottom Line
Obesity and decreased HDL cholesterol are more than casual acquaintances—they are co-conspirators in undermining heart health.
From impaired HDL production and altered enzyme activity to chronic inflammation and disrupted cholesterol transport, obesity throws a wrench in nearly every part of HDL’s function. But this is not a hopeless story.
With targeted lifestyle changes—like weight loss, regular exercise, and smarter food choices—you can flip the script. HDL does not just return; it comes back better equipped to protect your heart, clean up excess cholesterol, and reduce inflammation.
So while a healthy weight might not be the flashiest goal, it is one that quietly rebuilds the very molecules keeping your heart safe.
And that, in any medical playbook, is a win worth celebrating.
References: