Let’s face it: when it comes to obesity, the usual suspects—diet and exercise—often take center stage.
But there is a hidden player in the mix that does not get enough attention: your genes.
Yes, your inherited metabolism, shaped by genetic factors, plays a pivotal role in determining how your body processes food, stores fat, and uses energy.
In this article, we’ll explore the fascinating connection between inherited metabolism and obesity.
LeanAndFit research team shall also break down the science, dive into real-life examples, and uncover why some people seem to store fat no matter how much they exercise.
By the end, you will understand how genetics can tilt the scales and what you can do to regain control.
Article Index:
- What Is Inherited Metabolism?
- The Genetic Link: How Inherited Traits Influence Obesity
- Real-Life Example: Lisa’s Battle with Inherited Metabolism
- The Science Behind Metabolic Genes and Obesity
- How Hormones and Enzymes Play a Role
- Epigenetics: When Lifestyle Meets Genetics
- Long-Term Consequences of Ignoring Metabolic Factors
- FAQs on Inherited Metabolism in Obesity
- Conclusion: Balancing Genes with Lifestyle
What Is Inherited Metabolism?
Inherited metabolism refers to the unique way your body processes energy, shaped by the genetic blueprint passed down from your parents.
This genetic influence dictates your basal metabolic rate (BMR)—the number of calories your body burns at rest to maintain basic functions like breathing, digestion, and circulation.
Beyond BMR, inherited metabolism also affects how efficiently your body processes and uses nutrients like fats, proteins, and carbohydrates.
Think of inherited metabolism as the engine that drives your body’s energy needs.
Some people are born with a high-octane engine, burning through calories effortlessly, while others have a more fuel-efficient model, requiring fewer calories to function.
This difference means that two individuals eating identical diets and following the same exercise routine can experience vastly different outcomes in terms of weight.
For example, someone with a genetically slower metabolism may gain weight more easily than someone with a faster one, even if their caloric intake is identical.
This disparity can be attributed to genetic variations that affect factors like hormone regulation, fat storage, and energy expenditure.
While you cannot change your genetic blueprint, understanding its influence helps you tailor your lifestyle choices.
By optimizing diet and exercise to work with your metabolism, rather than against it, you can achieve healthier, more sustainable outcomes.
The Genetic Link: How Inherited Traits Influence Obesity
Genes play a pivotal role in obesity, setting the stage for how your body regulates appetite, stores fat, and manages energy.
Let’s meet the key genetic players involved in the battle of the bulge:
1. FTO Gene
Often referred to as the “fat gene,” the FTO gene has earned its reputation for good reason.
Variations in this gene affect how the brain regulates appetite and satiety, often leading to increased hunger and higher calorie consumption.
Studies show that people with certain FTO variations are more likely to crave calorie-dense foods and accumulate fat, especially in the abdominal region.
2. LEP Gene
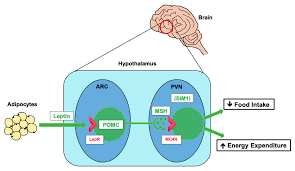
The LEP gene produces leptin, the hormone responsible for signaling fullness after a meal.
In individuals with genetic mutations in this gene, leptin signaling becomes impaired, leading to leptin resistance.
As a result, the brain does not recognize when the body has had enough to eat, making overeating a persistent challenge.
3. MC4R Gene
This gene influences the brain’s control over appetite and energy expenditure.
Mutations in the MC4R gene can impair the brain’s ability to regulate food intake, leading to heightened hunger and reduced calorie burning.
This imbalance significantly increases the risk of obesity.
Interplay of Genes and Environment
These genes do not operate in isolation—they interact with environmental factors like diet, physical activity, and stress.
For example, an individual with FTO variations who consumes a high-calorie diet may gain weight more rapidly than someone without the variation.
This dynamic highlights the complex web of genetic and lifestyle influences driving obesity.
Understanding these genetic factors is the first step in tailoring strategies to combat obesity effectively.
Real-Life Example: Lisa’s Battle with Inherited Metabolism
Lisa, a 35-year-old accountant, struggled with her weight for years despite following numerous diets and exercise plans.
Her frustration grew when her friends, who ate similar meals, seemed to stay slim effortlessly.
A genetic test revealed that Lisa had variations in the FTO and LEP genes, which explained her constant hunger and tendency to store fat.
Armed with this knowledge, she worked with a nutritionist to tailor her diet and bodyweight exercise routine.
By focusing on foods that kept her fuller longer and incorporating strength training, Lisa finally began to see results.
Lisa’s story highlights how understanding inherited metabolism can empower individuals to tackle obesity more effectively.
The Science Behind Metabolic Genes and Obesity
Scientific research has shed light on the genetic underpinnings of metabolism and obesity:
- “Genetic Factors in Obesity” (Nature Reviews Endocrinology, 2020): This study identified over 400 genes linked to body weight regulation, including those that influence appetite, fat storage, and energy expenditure.
- “Role of FTO Gene Variants in Obesity” (Diabetes, 2017): Found that individuals with specific FTO gene variations had a 20-30% higher risk of obesity.
- “Leptin Resistance and Obesity” (Journal of Clinical Investigation, 2019): Highlighted how genetic mutations in the LEP gene disrupt the brain’s ability to regulate hunger, leading to overeating.
These studies confirm that genetics play a significant role in obesity, shaping how the body processes energy and responds to food.
How Hormones and Enzymes Play a Role
Your inherited metabolism is not solely determined by your genes—it is also heavily influenced by hormones and enzymes that regulate energy balance.
These biochemical players are crucial in controlling appetite, fat storage, and energy use.
When their balance is disrupted due to genetic predispositions, maintaining a healthy weight becomes a challenging uphill battle.
Leptin: The Satiety Hormone
Leptin signals your brain when you are full, acting as a brake on your appetite.
However, genetic mutations can lead to leptin resistance, where the brain fails to receive these fullness signals.
As a result, hunger persists even after eating, promoting overeating and weight gain.
Ghrelin: The Hunger Hormone
Ghrelin works as the counterpart to leptin, stimulating appetite and encouraging fat storage.
Certain genetic factors can elevate ghrelin levels, intensifying hunger pangs and making portion control more difficult.
This hormonal imbalance creates a perfect storm for weight gain.
Lipoprotein Lipase (LPL): The Fat Manager
This enzyme is responsible for storing and releasing fat in your body.
Genetic profiles with higher LPL activity tend to store fat more efficiently, particularly in adipose tissues.
While this might have been an evolutionary advantage, in today’s calorie-rich environment, it contributes to obesity.
When these hormones and enzymes are disrupted due to genetics, the body’s ability to regulate energy balance falters.
This highlights the importance of understanding inherited metabolism to craft effective strategies for weight management and overall health.
Epigenetics: When Lifestyle Meets Genetics
Here is where things get really fascinating.
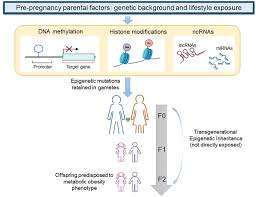
While your genes provide the blueprint, epigenetics—the science of how lifestyle factors influence gene expression—has a starring role in shaping outcomes like obesity.
Essentially, epigenetics acts as a dimmer switch, turning genes on or off depending on environmental inputs.
For Example:
- Diet: Consuming a high-fat, high-sugar diet can activate genes linked to fat storage, making weight gain more likely. Conversely, a balanced diet rich in whole foods can counteract genetic predispositions by reducing inflammation and improving metabolism.
- Exercise: Regular physical activity does not just burn calories; it also boosts the expression of genes that promote fat burning while suppressing those associated with weight gain and fat storage.
The Science Behind It:
A study published in Obesity Reviews (2019) revealed that individuals with a genetic predisposition to obesity could lower their risk by 40% through consistent healthy lifestyle choices.
This underscores the idea that while you cannot change your genes, you can influence how they behave.
The takeaway?
Your genetic predisposition is not your destiny.
By making conscious lifestyle decisions, you can rewrite the story your genes want to tell, keeping obesity at bay despite the odds.
Long-Term Consequences of Ignoring Metabolic Factors
Failing to address inherited metabolic factors can have serious and far-reaching consequences, impacting not only your immediate health but also future generations.
Let’s dive into the potential risks:
Chronic Diseases:
Obesity, fueled by genetic predispositions, significantly raises the risk of chronic conditions like type 2 diabetes, heart disease, and hypertension.
These diseases not only reduce quality of life but also place a significant strain on healthcare systems and personal finances.
Mental Health Struggles:
The constant battle with genetic tendencies toward weight gain can take a toll on mental health.
The frustration of managing a predisposed slow metabolism or insatiable appetite often leads to stress, anxiety, and depression, creating a cycle that’s difficult to break.
Intergenerational Impact:
Obesity-related genes don’t stop with you—they can be passed down to future generations.
Children of parents with metabolic predispositions are at a higher risk of developing obesity, perpetuating the cycle across family lines.
Understanding these factors and addressing them early is key.
Proactive steps, such as tailored diets, regular physical activity, and stress management, can help mitigate these risks.
By doing so, individuals can improve their health outcomes and break the cycle of inherited metabolic challenges.
FAQs on Inherited Metabolism in Obesity
Q-1: How much of body weight is inherited—and why do estimates vary so widely?
A-1: A substantial share of BMI is heritable, but the percentage shifts with context. Genes set a baseline for appetite, energy use, and fat storage, while environment—food access, sleep, stress, movement—decides how strongly those genes “speak.” In settings loaded with calorie-dense food and low activity, genetic effects appear larger; in supportive environments, they appear smaller.
Q-2: What does “polygenic risk” really predict about my future body weight?
A-2: Polygenic scores combine thousands of tiny DNA influences. They can flag earlier-than-average fat gain or an easier time regaining weight after diets, but they are probabilistic, not destiny. Their real value is timing: they help identify who benefits most from early habits like higher-protein meals, resistance training, and consistent sleep—before weight climbs.
Q-3: Which single-gene pathways most clearly shift inherited appetite and energy balance?
A-3: The leptin–melanocortin pathway is the clearest example. Variants that weaken signaling through this circuit often heighten hunger, dull fullness cues, and alter autonomic tone. While rare, these changes show how a single pathway can move both intake and energy use, explaining severe, early-onset weight gain in some families.
Q-4: How do common “fat gene” variants change calorie burn, not just appetite?
A-4: Some DNA changes bias precursor cells toward storing energy rather than burning it. They tip the balance away from mitochondria-rich, heat-generating fat cells and toward energy-saving ones. The effect is subtle: you won’t “gain weight from air,” but you may need tighter habits to maintain leanness compared with someone without that bias.
Q-5: Is mitochondrial inheritance part of the obesity story?
A-5: Mitochondria—the cell’s engines—are inherited from the mother and influence how efficiently we turn fuel into energy. Certain maternal-line patterns are linked with differences in metabolic efficiency. The effects are modest and population-specific, but they add another layer to why weight regulation can “run in families.”
Q-6: Can inherited metabolism be “programmed” before birth?
A-6: Yes. Beyond DNA, conditions in the womb—like maternal glucose and weight—can leave epigenetic marks that shape a child’s later insulin sensitivity, appetite signaling, and fat storage. This intergenerational programming stacks on top of genetic risk, which is why healthy gestational weight gain and early-life nutrition have outsized long-term benefits.
Takeaway: Inherited metabolism sets starting conditions, not a final outcome. Polygenes, rare appetite-pathway variants, mitochondrial traits, and prenatal programming nudge energy balance. The practical response is precision prevention: earlier monitoring, protein-forward meals, regular resistance training, daily movement, and consistent sleep—especially when family history suggests higher inherited risk.
Takeaway: Balancing Genes with Lifestyle
Inherited metabolism plays a significant role in shaping obesity risk, but it is not a life sentence.
While genetic predispositions create challenges, they can be managed through targeted lifestyle changes and personalized interventions.
Awareness is the first step.
Tools like genetic testing, combined with professional guidance, can help individuals understand their unique metabolic profile.
By focusing on balanced nutrition, regular exercise, and stress management, it is possible to counteract the effects of inherited metabolism and achieve sustainable weight management.
So, the next time you are tempted to blame yourself for weight struggles, remember: it is not just willpower—it is your inherited metabolism.
Armed with knowledge and a plan, you can tip the scales in your favor.
References: