Obesity is often associated with common health risks like diabetes and joint problems, but what about its hidden impact on the heart?
Cardiac overload, a condition where the heart is overworked due to increased demands from the body, is one of the lesser-discussed consequences of obesity.
As your body size increases, so does the strain on your heart, leading to various complications that could become life-threatening if left unchecked.
In this article, leanandfit.info will explore how obesity contributes to cardiac overload, the signs and symptoms to watch for, and ways to address this issue before it spirals out of control.
“Is Cardiac Overload the Hidden Danger of Obesity” Article Index:
- What is Cardiac Overload?
- Cardiac Volume Overload and Obesity
- Pressure Overload in the Heart
- Cardiac Fluid Overload: Causes and Risks
- Signs of Cardiac Overload
- Cardiac Iron Overload and Obesity
- Can Cardiac Overload be Reversed?
- FAQs on Cardiac Overload and Obesity
- Conclusion: Is Cardiac Overload the Hidden Danger of Obesity?
What is Cardiac Overload?
Cardiac overload occurs when the heart is forced to work harder than normal to pump blood throughout the body.
This can happen in two forms: pressure overload and volume overload. In both cases, the heart becomes strained and may begin to enlarge or weaken over time.
Obesity, with its added body mass and increased metabolic demands, can lead to cardiac overload, placing significant stress on the cardiovascular system.
Scientific research published in The Journal of Clinical Investigation confirms that obesity is a major contributing factor to heart disease due to this overload mechanism.
Cardiac Volume Overload and Obesity
In the context of obesity, cardiac volume overload occurs when the heart is forced to manage an increased blood volume due to excess body fat.
As body fat increases, so does the body’s total blood volume, placing additional demand on the heart. Imagine your heart as a pump designed for a specific capacity—when the volume exceeds what it’s built for, it must work harder to keep up.
In someone with a healthier weight, this demand is manageable, but in individuals with obesity, the constant overwork can weaken heart muscles over time, increasing the risk of conditions like heart failure.
This risk is significantly higher when leptin resistance is also present.
Leptin, a hormone primarily involved in regulating appetite and metabolism, also affects cardiovascular health. When leptin signaling fails, it promotes chronic inflammation and further stresses the heart.
A study in The American Journal of Cardiology confirmed that obesity-induced cardiac volume overload directly accelerates heart disease, especially in individuals with high body mass index (BMI).
Persistent strain on the heart leads to left ventricular hypertrophy (enlargement of the heart’s main pumping chamber), which can result in arrhythmias and long-term heart failure if left unchecked.
Recognizing and managing cardiac volume overload early is crucial to preserving heart function.
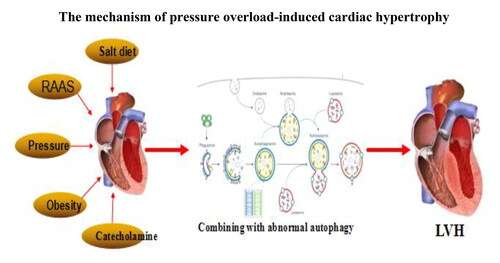
Pressure Overload in the Heart
Pressure overload in the heart is another type of strain associated with obesity. When blood pressure increases due to obesity, the heart has to pump against greater resistance in the arteries.
This type of overload makes the heart work harder to move blood, leading to thickening of the heart muscles, especially in the left ventricle.
Over time, this thickening can result in a loss of flexibility, making the heart less efficient at pumping blood. This increases Atherosclerosis Risk in Obesity.
According to the Journal of Hypertension, people who are obese are significantly more likely to experience pressure overload, leading to long-term cardiovascular complications.
Cardiac Fluid Overload: Causes and Risks
In some cases, obesity can lead to cardiac fluid overload, a condition where the body retains excess fluids.
When this happens, the heart has to pump not only an increased blood volume but also manage the additional fluid, which puts more strain on the heart.
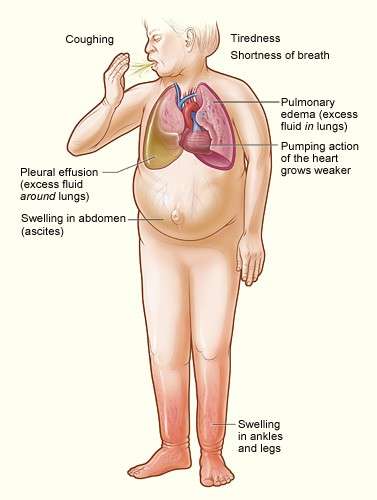
This often results in swelling (edema) in the legs, ankles, and abdomen. Cardiac fluid overload can be a precursor to congestive heart failure if not managed promptly.
Health professionals often use diagnostic codes like cardiac volume overload ICD-10 to classify and treat this condition. It has also been ascertained that obesity impacts your cardiovascular health.
Signs of Cardiac Overload
Recognizing signs of cardiac overload is crucial for early intervention and preventing serious heart conditions.
Common symptoms include shortness of breath during physical activity or even at rest, persistent fatigue, chest pain or tightness, and swelling in the lower extremities, particularly the ankles and feet.
These signs indicate that the heart is struggling to pump blood efficiently, which can lead to fluid retention and increased pressure on the cardiovascular system.
If left untreated, cardiac overload can progress to heart failure or other life-threatening conditions.
For example, an individual with obesity may experience frequent shortness of breath and assume it’s due to poor fitness or weight alone, overlooking the possibility of an underlying cardiac problem.
According to the American Heart Association, early recognition of these symptoms can significantly improve outcomes, particularly for individuals with risk factors like hypertension, obesity, and diabetes.
Scientific studies, such as one published in Circulation, highlight that heart failure patients who receive treatment at the early stages of cardiac overload have a far better prognosis than those diagnosed at advanced stages.
Identifying warning signs early allows for interventions like lifestyle changes, medications, and improved blood pressure management, ultimately reducing the risk of long-term heart complications.
Cardiac Iron Overload and Obesity
Let’s talk about another sneaky culprit behind heart problems in obese individuals—cardiac iron overload.
Sounds fancy, but it is basically what happens when too much iron builds up in the heart tissue.
While your body needs iron to survive (hello, red blood cells), too much of it in the wrong place can spell trouble.
Excess iron can cause inflammation and damage in the heart, eventually leading to heart dysfunction or, worse, heart failure.
Now, you might think cardiac iron overload is something only people with genetic conditions like hemochromatosis need to worry about.
But here is the kicker—research suggests that individuals with obesity may experience altered iron metabolism, leading to increased iron deposition in the heart.
Essentially, the body’s iron-regulating system gets thrown out of whack, piling even more stress on an already overworked heart.
Think of it this way: obesity is like carrying an overpacked suitcase on a long journey, and cardiac iron overload is that extra unnecessary weight stuffed in at the last minute.
The result?
A heart that is tired and struggling to keep up.
Studies published in Cardiology Journal emphasize that addressing altered iron metabolism could be key to improving cardiac outcomes in people with obesity.
Can Cardiac Overload be Reversed?
The good news is that cardiac overload is not necessarily a one-way street.
Lifestyle changes, such as weight loss, increased physical activity, and improved dietary habits, can reduce the strain on the heart.
Medications to manage blood pressure, reduce fluid retention, and control cholesterol levels can also help.
In severe cases, medical interventions such as bariatric surgery may be considered to reduce obesity-related heart strain.
According to a study published in Circulation, weight loss significantly reduces the risk of developing heart failure, even in people who already have some degree of cardiac overload.
FAQs on Cardiac Overload and Obesity
Q-1: Why does obesity quietly overload the heart even before blood pressure is “high”?
A-1: Extra body mass requires more blood flow to supply larger fat and muscle depots. The body expands total blood volume and cardiac output to keep up, so the heart pumps harder every minute—24/7. Over months to years this “always-on” demand triggers chamber enlargement and wall thickening, especially of the left ventricle, nudging you toward diastolic dysfunction long before a routine cuff ever flags hypertension.
Q-2: How does belly fat specifically strain the heart differently from weight elsewhere?
A-2: Visceral and epicardial fat bathe the heart and coronary vessels in inflammatory signals. Epicardial fat sits millimeters from the myocardium and shares microcirculation, so its cytokines can stiffen the heart muscle and impair relaxation locally. That combo—systemic volume load plus local inflammation—sets the stage for the “obesity cardiomyopathy” pattern and helps explain shortness of breath despite normal coronary angiograms.
Q-3: Can obesity mask heart failure by lowering the very biomarkers doctors rely on?
A-3: Yes. Natriuretic peptides (like BNP) are paradoxically lower in many people with obesity, even when filling pressures are high. A “normal” BNP can therefore under-call early heart failure with preserved ejection fraction. Clinicians often lean more on symptoms, imaging (diastolic indices, left atrial size), and exercise testing in higher-BMI patients to avoid missing occult cardiac overload.
Q-4: Why do sleep issues in obesity amplify cardiac overload at night?
A-4: Obstructive sleep apnea causes repeated oxygen dips and pressure swings in the chest. Each event spikes sympathetic drive and blood pressure, stressing the heart and pulmonary circulation. Over time, this raises risks of atrial fibrillation, right-sided strain, and resistant hypertension—meaning the heart works hardest during the very hours it should be recovering.
Q-5: If weight loss is gradual, can the heart actually “reverse” overload?
A-5: Often, yes. Even modest, sustained loss reduces blood volume, resting heart rate, and left-ventricular mass, easing diastolic pressures. Add aerobic training and light resistance work: arteries relax better, sleep improves, and natriuretic peptide signaling rebounds. Practical markers of improvement include lower resting pulse, easier stair climbing, shrinking waist, and echocardiogram signs of softer filling pressures—proof the heart is off the emergency shift.
Conclusion: Is Cardiac Overload the Hidden Danger of Obesity?
So, is cardiac overload the hidden danger of obesity?
Absolutely. While obesity has long been recognized for its role in contributing to diabetes, joint problems, and sleep apnea, its impact on the heart—particularly through cardiac overload—remains under-discussed.
Obesity places enormous stress on the heart, whether through cardiac volume overload, pressure overload in the heart, or even more specific issues like cardiac iron overload. I have shed countless pounds of unwanted body fat drinking delicious smoothies.
The signs of cardiac overload may be subtle at first, but recognizing them early and addressing the root cause—obesity—can lead to better outcomes.
The solution lies in early intervention, lifestyle changes, and medical management to reduce the heart’s workload and improve overall health.
References: