Obesity and insulin resistance are like two sides of the same coin, each contributing to a vicious cycle of health complications.
While obesity is well-known for its visible effects, such as weight gain, insulin resistance operates more subtly but poses significant dangers.
Together, these conditions form a dangerous duo, leading to various health issues, including type 2 diabetes, cardiovascular diseases, and metabolic syndrome.
But what are the hidden health dangers of insulin resistance and obesity, and how do they impact your overall well-being?
In this article, leanandfit.info shall explore the intricate relationship between insulin resistance and obesity, how they affect your body, and the long-term consequences if left untreated.
Article Index
- Insulin Resistance and Obesity: The Connection
- Insulin Resistance Obesity: A Cycle of Health Risks
- Abdominal Obesity and Insulin Resistance: The Dangerous Fat
- Insulin Resistance Overweight: When the Scale Tells More Than Just Weight
- FAQS on Insulin Resistance and Obesity
- Conclusion: Unveiling the Hidden Dangers
Insulin Resistance and Obesity: The Connection
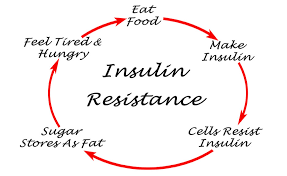
The relationship between insulin resistance and obesity is complex and deeply intertwined. Insulin resistance occurs when the body’s cells become less responsive to insulin, a hormone produced by the pancreas to regulate blood sugar levels.
As a result, the body requires more insulin to maintain normal glucose levels, leading to elevated blood insulin and blood sugar. Over time, this imbalance can lead to type 2 diabetes.
As per LeanAndFit, “Obesity, particularly visceral fat (fat around the organs), exacerbates insulin resistance. This excess fat releases free fatty acids into the bloodstream, which interfere with insulin’s ability to signal cells to absorb glucose”.
In short, the more body fat you have, especially around the abdomen, the higher your risk of developing insulin resistance. This creates a cycle where insulin resistance leads to further weight gain, and weight gain increases insulin resistance.
Insulin Resistance Obesity: A Cycle of Health Risks
The term insulin resistance obesity refers to the situation where obesity and insulin resistance coexist, creating a cycle of health risks.
Studies have shown that being obese increases the risk of developing insulin resistance, and in turn, insulin resistance makes it harder to lose weight. This is because insulin plays a crucial role in how your body stores and uses energy.
When insulin function is impaired, your body stores more fat and burns fewer calories, leading to calorie surplus, making weight loss difficult.
The health risks do not stop there. Individuals with both obesity and insulin resistance are at a much higher risk of developing metabolic syndrome, a cluster of conditions that include high blood pressure, high cholesterol, and high blood sugar.
These factors increase the likelihood of developing cardiovascular diseases such as heart attacks and strokes. Furthermore, insulin resistance is closely linked to chronic inflammation, which has been identified as a root cause of many obesity-related diseases.
Abdominal Obesity and Insulin Resistance: The Dangerous Fat
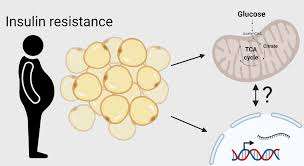
One of the most dangerous types of fat is abdominal obesity or visceral fat. Unlike subcutaneous fat (the fat under the skin), visceral fat surrounds internal organs and is more metabolically active.
This means it has a more significant impact on the body’s hormonal balance, especially when it comes to insulin regulation.
Abdominal obesity and insulin resistance are tightly connected, with research showing that individuals with a higher amount of visceral fat are more likely to develop insulin resistance.
This is due to the fat cells releasing inflammatory chemicals known as cytokines, which interfere with the insulin signaling pathway.
Moreover, abdominal fat increases the release of free fatty acids, further aggravating insulin resistance.
This specific type of fat is considered a primary factor in developing type 2 diabetes and other metabolic disorders, making it one of the most dangerous consequences of obesity.

Insulin Resistance Overweight: When the Scale Tells More Than Just Weight
Understanding that weight alone does not paint the full picture of health is crucial, especially when considering insulin resistance. Here’s a friendly breakdown to shed light on this important topic:
Weight Isn’t Everything:
- Many individuals may not be classified as obese based on traditional metrics like Body Mass Index (BMI) but can still face significant metabolic challenges due to insulin resistance.
- Even if weight appears “normal,” underlying health concerns such as high blood sugar levels or metabolic dysfunction can still be present.
The Role of Visceral Fat:
- Visceral fat is stored deep within the abdominal cavity, surrounding vital organs.
- Even with a healthy BMI, excess visceral fat can pose similar health risks to obesity.
- According to the Mayo Clinic, visceral fat is metabolically active and can interfere with insulin function, increasing the risk of diabetes and heart disease.
Modest Weight Gain Matters:
- Even a small amount of weight gain can trigger insulin resistance.
- A study published in Diabetes Care found that gaining just a few pounds can lead to increased insulin levels and reduced insulin sensitivity.
- This highlights why monitoring body composition, rather than just weight, is important.
Silent Progression of Insulin Resistance:
- Insulin resistance can develop even if the scale doesn’t show a drastic increase.
- According to Harvard Medical School, insulin resistance is often asymptomatic in the early stages, meaning regular health check-ups are necessary.
The Concept of Normal Weight Obesity (NWO):
- Normal Weight Obesity (NWO) refers to individuals with a normal BMI but a high body fat percentage, particularly visceral fat.
- The Cleveland Clinic states that people with NWO face a higher risk of metabolic syndrome and type 2 diabetes, similar to those with obesity.
Importance of Body Composition:
- Body composition, including fat-to-muscle ratio, is a better health indicator than weight alone.
- The National Institutes of Health recommends using tools like body fat percentage analysis and waist circumference measurements for a more accurate assessment of health risks.
Lifestyle Factors Play a Role:
- Poor diet, sedentary behavior, and genetics all contribute to insulin resistance.
- Research from the American Diabetes Association highlights that regular exercise and a balanced diet can improve insulin sensitivity, even in individuals who are not overweight.
Monitoring and Early Detection:
- Routine health screenings, including fasting glucose and insulin tests, help detect early signs of insulin resistance.
- Johns Hopkins Medicine suggests that early detection allows for interventions that can prevent progression to type 2 diabetes.
Individualized Health Assessments:
- A personalized health assessment from a healthcare provider can give a more detailed understanding of metabolic health.
- The World Health Organization emphasizes that a one-size-fits-all approach to weight management may not be effective, and personalized care is key.
Holistic Health Perspective:
- Sleep, stress management, and mental well-being play a crucial role in insulin sensitivity.
- According to the National Sleep Foundation, poor sleep is directly linked to increased insulin resistance and a higher risk of metabolic disorders.
Weight alone is not the best indicator of health. By focusing on body composition, visceral fat, and overall lifestyle, individuals can gain a better understanding of their metabolic health and take proactive steps to prevent insulin resistance.
FAQs on Insulin Resistance and Obesity
Unveiling the Hidden Dangers
So, is insulin resistance and obesity a hidden health danger?
The answer is a resounding yes.
Both insulin resistance and obesity contribute to a dangerous feedback loop that significantly increases the risk of developing severe health conditions, including type 2 diabetes, cardiovascular disease such as atherosclerosis, and metabolic syndrome.
Moreover, abdominal obesity makes the situation even more precarious, as it accelerates the development of insulin resistance and amplifies the risk of related complications.
However, the good news is that insulin resistance and obesity are not irreversible. Weight loss, even in modest amounts, can significantly improve insulin sensitivity.
Regular physical activity, a balanced smoothie based fat loss diet, and stress management are effective ways to combat both obesity and insulin resistance. In many cases, addressing lifestyle factors can reverse the cycle and lead to improved health outcomes.
By understanding the deep connection between insulin resistance and obesity, and by taking proactive steps to manage these conditions, you can significantly reduce your risk of long-term health issues.
The hidden dangers may be significant, but with knowledge and action, they can be mitigated and, in many cases, avoided altogether.
References: