Obesity is often associated with physical health issues like diabetes and heart disease, but its impact on brain structure is an area of growing concern.
Scientific research reveals that excessive weight gain can lead to structural and functional changes in the brain, affecting cognitive performance, memory, and emotional regulation.
In this article, leanandfit.info will explore how and why obesity alters brain structure, focusing on the underlying mechanisms, affected regions, and the long-term implications of these changes.
Article Index
- Introduction to Obesity and Brain Structure
- Mechanisms Linking Obesity to Brain Changes
- 2.1. Inflammation and Neurodegeneration
- 2.2. Insulin Resistance and Cognitive Decline
- Brain Regions Affected by Obesity
- 3.1. Prefrontal Cortex and Executive Function
- 3.2. Hippocampus and Memory Impairment
- 3.3. Hypothalamus and Appetite Regulation
- Real-Life Impacts of Obesity on Brain Health
- Scientific Evidence Supporting Obesity’s Role in Brain Alterations
- FAQs on Obesity and Brain Structure
- Conclusion: Understanding the Brain-Obesity Connection
Introduction to Obesity and Brain Structure
Obesity, marked by the excessive accumulation of body fat, has become a global health crisis with significant implications for both physical and mental well-being.
While its effects on cardiovascular and metabolic health are widely discussed, its impact on brain structure often remains overlooked.
Emerging research reveals that obesity can profoundly alter brain volume, reduce gray matter density, and disrupt neural connections.
These changes contribute to cognitive impairments, emotional dysregulation, and even an increased risk of neurodegenerative diseases.
Key Areas of Exploration:
- Biological Mechanisms: How inflammation, insulin resistance, and hormonal imbalances affect brain health.
- Affected Brain Regions: Specific areas such as the hippocampus, prefrontal cortex, and hypothalamus are particularly vulnerable.
- Real-Life Impacts: Practical examples of how these changes manifest, from memory lapses to impulse control difficulties.
This article will explore these facets in detail, shedding light on the critical yet underappreciated relationship between obesity and brain health.
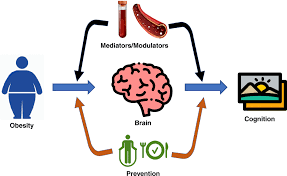
Mechanisms Linking Obesity to Brain Changes
Obesity rewires the brain, courtesy of inflammation, insulin resistance, and hormonal chaos—turning neurons into couch potatoes while shrinking gray matter’s real estate.
Inflammation and Neurodegeneration:
Obesity sets off low-grade chronic inflammation, a systemic condition characterized by increased levels of pro-inflammatory molecules such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6).
These inflammatory cytokines can cross the blood-brain barrier, triggering neuroinflammation. Prolonged neuroinflammation disrupts neuronal signaling, accelerates neuronal damage, and contributes to cognitive decline and mood disorders.
Effects on Brain Health:
- Gray Matter Reduction: Chronic inflammation linked to obesity has been associated with atrophy in brain regions responsible for memory, decision-making, and impulse control, such as the hippocampus and prefrontal cortex.
- Accelerated Aging: Neuroinflammation hastens brain aging processes, impairing cognitive functions over time.
Supporting Evidence:
A study published in Nature Reviews Neuroscience (Miller & Spencer, 2014) found that obesity-induced inflammation leads to reduced gray matter volume in essential brain areas.
These findings underscore the dual role of obesity in systemic and neurological health decline, emphasizing the importance of addressing inflammation to preserve brain function.
Insulin Resistance and Cognitive Decline
Obesity frequently leads to insulin resistance, a condition in which the body’s cells become less responsive to insulin.
While this is widely known for its effects on glucose metabolism, it also has profound implications for brain health.
Insulin plays a critical role in brain functions such as learning, memory, and synaptic plasticity. In obese individuals, impaired insulin signaling in the brain exacerbates cognitive decline, particularly in regions like the hippocampus.
Impact of Insulin Resistance:
- Reduced Synaptic Plasticity: Impaired insulin signaling affects the brain’s ability to form and reorganize synaptic connections, essential for learning and memory.
- Compromised Hippocampal Function: The hippocampus, a key area for memory processing, becomes less effective, contributing to memory deficits and cognitive impairment.
Research published in The Journal of Clinical Investigation (Arnold et al., 2018) found that insulin resistance correlates with reduced brain volume, particularly in the prefrontal cortex and hippocampus.
These findings emphasize how metabolic dysfunctions in obesity can significantly compromise brain health, highlighting the need to address insulin resistance for both physical and cognitive well-being.
Brain Regions Affected by Obesity
Obesity impacts key brain regions like the hippocampus, prefrontal cortex, and hypothalamus, shrinking gray matter and disrupting memory, decision-making, and appetite control.
Prefrontal Cortex and Executive Function
The prefrontal cortex, responsible for decision-making and impulse control, is particularly vulnerable to the effects of obesity.
Reduced gray matter in this region impairs executive function, leading to difficulties in planning, attention, and self-regulation.
Example:
John, a 45-year-old manager, struggled with overeating and found it challenging to focus on work tasks.
MRI scans revealed reduced gray matter density in his prefrontal cortex, a common finding in individuals with obesity.
Hippocampus and Memory Impairment
The hippocampus, a vital brain region responsible for memory formation and spatial navigation, is particularly vulnerable to the effects of obesity.
Chronic inflammation and insulin resistance, common in obesity, impair hippocampal function and structure.
Studies reveal that obesity reduces hippocampal volume, correlating with memory decline and cognitive impairments.
Supporting Evidence:
A study published in Brain Imaging and Behavior (Kharabian Masouleh et al., 2018) demonstrated that individuals with higher body mass index (BMI) exhibited significantly smaller hippocampal volumes.
This reduction was directly associated with poorer memory performance, emphasizing the critical impact of obesity on cognitive health and brain structure.
Hypothalamus and Appetite Regulation
The hypothalamus, a vital brain region responsible for regulating hunger and satiety, undergoes significant structural and functional alterations in individuals with obesity.
Chronic overeating induces inflammation in the hypothalamus, damaging neurons that play a key role in appetite control.
This neural disruption creates a vicious cycle where the brain struggles to signal fullness, leading to continued overeating.
Key Impacts:
- Persistent Hunger Signals: Despite adequate or excess energy stores, the brain sends signals for continued food intake.
- Leptin Resistance: The hypothalamus becomes less sensitive to leptin, a hormone produced by fat cells that typically suppresses appetite and promotes energy balance. This insensitivity undermines the body’s natural mechanisms for maintaining a healthy weight.
Scientific evidence supports these findings:
A study in The Journal of Clinical Investigation (Thaler et al., 2012) highlighted hypothalamic inflammation as an early consequence of high-fat diets, showing measurable neuron loss and impaired signaling.
Understanding these changes underscores how obesity disrupts brain mechanisms, reinforcing the cycle of overeating and weight gain.
Real-Life Impacts of Obesity on Brain Health
We shall be listing out two real life examples on this very topic. This has been done so as to share real life data with you. So, let’s take a closer look:
Emily’s Memory Challenges
Emily, a 40-year-old marketing professional, found herself frequently forgetting appointments and struggling to recall recent conversations.
Her BMI of 36 classified her as obese, prompting her to seek medical advice. Neuroimaging revealed a significant reduction in her hippocampal volume, a hallmark of obesity-related brain changes.
Research from Brain Imaging and Behavior (Kharabian Masouleh et al., 2018) supports these findings, showing that higher BMI correlates with hippocampal atrophy and memory deficits.
Additionally, chronic inflammation and insulin resistance were identified as contributing factors, further exacerbating her cognitive decline.
Jake’s Struggle with Food Cravings
Jake, a 45-year-old software engineer, noticed an inability to resist unhealthy snacks, leading to frequent binge-eating episodes.
Despite knowing the consequences, he felt powerless to control his cravings. MRI scans revealed reduced gray matter in his prefrontal cortex, an area responsible for decision-making and impulse control.
Studies, such as one published in Nature Reviews Neuroscience (Miller & Spencer, 2014), link obesity-induced inflammation to neurodegeneration in this critical brain region.
Jake’s experience highlights how obesity disrupts neural circuits involved in self-regulation, making it harder to break the cycle of overeating.
These real-life examples illustrate the profound effects obesity can have on memory and impulse control, reinforcing the importance of addressing its impact on brain health.
Scientific Evidence Supporting Obesity’s Role in Brain Alterations
Here are 4 scientific research studies that link brain damage to obesity. Let us walk you through each of these in brief:
Study 1: Nature Reviews Neuroscience (Miller & Spencer, 2014)
This foundational study illuminated the connection between obesity-induced inflammation and neurodegeneration.
It emphasized how elevated levels of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), contribute to the reduction of gray matter volume.
The findings linked chronic neuroinflammation to impaired brain function.
Study 2: The Journal of Clinical Investigation (Arnold et al., 2018)
This research explored how insulin resistance, a hallmark of obesity, affects the brain.
The study established a direct relationship between insulin dysfunction and hippocampal impairment, offering insight into the mechanisms driving obesity-related cognitive decline.
Study 3: Brain Imaging and Behavior (Kharabian Masouleh et al., 2018)
Researchers found that individuals with a higher body mass index (BMI) had significantly reduced hippocampal volume.
This study highlighted the connection between BMI and memory deficits, shedding light on the structural brain changes caused by obesity.
Study 4: Endocrine Reviews (Schwartz et al., 2017)
This study focused on hypothalamic damage resulting from overeating.
It explained how this damage disrupts appetite regulation, perpetuating the cycle of weight gain.
The findings demonstrated the critical role of hypothalamic health in managing obesity.
FAQs on Obesity and Brain Structure
Q-1: Which brain structures show the most consistent changes with higher body fat?
A-1: The strongest pattern is thinner cerebral cortex across widespread regions, with more variable effects on surface area. Subcortical differences can also appear in memory- and emotion-related areas such as the hippocampus and amygdala. In short, obesity relates more to microstructural features (like cortical thickness) than to overall brain size alone.
Q-2: How does obesity affect the brain’s wiring (white matter)?
A-2: Measures of white-matter integrity often show small but meaningful reductions—especially in tracts involved in attention and self-control, like the front of the corpus callosum. These changes suggest altered myelin or axonal organization and align with slower processing speed and less efficient executive function in some individuals.
Q-3: What biological pathways could connect excess adiposity to structural brain change?
A-3: Visceral fat promotes chronic, low-grade inflammation that can disturb the blood–brain barrier and heighten immune signaling inside the brain. Metabolic stress in hypothalamic regions that regulate appetite and energy balance may further drive local remodeling, linking body-wide inflammation and insulin resistance to neural structure.
Q-4: Are these changes uniform, or do certain networks look more vulnerable?
A-4: They’re not uniform. Circuits that govern reward, interoception (body-signal awareness), and cognitive control show particular sensitivity. This network pattern mirrors behaviors relevant to weight regulation—greater response to food cues, difficulty delaying rewards, and variable self-regulation—suggesting targeted circuit susceptibility rather than global atrophy.
Q-5: Can improving metabolic health nudge brain structure in a positive direction?
A-5: Early intervention studies are encouraging. Weight loss, better cardiorespiratory fitness, and glucose control have been linked to preservation—or modest gains—in cortical or hippocampal measures. The effects are not dramatic, but they point to brain plasticity when vascular strain, inflammation, and insulin resistance improve over months to years.
Q-6: Does fat distribution matter as much as total weight for the brain?
A-6: Yes. Central (visceral) adiposity—often captured by waist-to-hip ratio—tends to track more strongly with adverse brain markers than BMI alone. In midlife, higher visceral fat is associated with smaller gray-matter volumes and more white-matter lesions later on. That’s why strategies that specifically reduce abdominal fat—nutrition quality, resistance plus aerobic training, sleep regularity—may offer outsized brain benefits compared with weight loss that spares central fat.

Takeaway: Understanding the Brain-Obesity Connection
Obesity’s impact on brain structure is profound, affecting critical areas like the prefrontal cortex, hippocampus, and hypothalamus.
The interplay of inflammation, insulin resistance, and neuronal damage underscores the systemic nature of this condition. Obesity reduces your lung capacity thereby leaving you gasping for breath.
By understanding these mechanisms, we can better appreciate the importance of addressing obesity not just as a physical health issue but as a factor in cognitive and emotional well-being.
Advancements in neuroscience and endocrinology offer hope for mitigating these effects, emphasizing the need for early intervention and holistic approaches to weight management.
Recognizing the brain-obesity connection is a vital step in fostering a healthier future for individuals affected by obesity.
References: