Leptin resistance is a critical yet often overlooked factor contributing to obesity and weight management struggles.
While leptin, a hormone produced by fat cells, plays a pivotal role in regulating hunger and metabolism, its effectiveness can diminish due to resistance.
This condition, known as leptin resistance, prevents the brain from recognizing the body’s fat stores, leading to overeating and difficulty losing weight.
This article by LeanAndFit research staff explores the science behind leptin resistance, its impact on weight loss, and possible solutions to tackle this issue.
“How Leptin Resistance is Ruining Your Weight Loss Efforts” Article Index:
- What is Leptin and Why is it Important?
- Understanding Leptin Resistance
- Causes and Symptoms of Leptin Resistance
- How Leptin Resistance Affects Weight Loss
- Diagnosing Leptin Resistance
- Effective Strategies to Manage Leptin Resistance
- FAQs On Leptin Resistance and Body Fat
- Conclusion: Can Leptin Resistance be Reversed?
What is Leptin and Why is it Important?
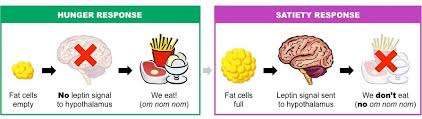
Leptin is a hormone produced by adipose (fat) tissue that signals the brain to regulate hunger and energy balance.
When fat stores are sufficient, leptin levels increase, signaling the brain to reduce appetite and increase energy expenditure.
Conversely, low leptin levels indicate energy deficiency, prompting the brain to increase hunger and reduce metabolism to conserve energy.
This feedback loop is crucial for maintaining a healthy weight and preventing obesity.
Understanding Leptin Resistance
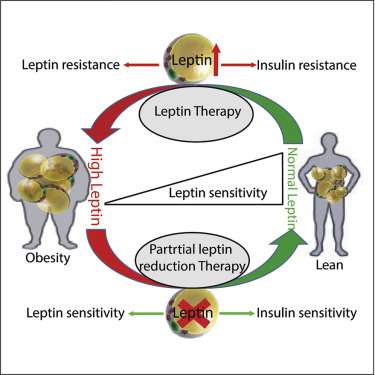
Leptin resistance is a condition where the brain no longer responds properly to leptin, the hormone responsible for regulating hunger and energy balance. In a healthy system, leptin signals the brain that the body has sufficient fat stores, suppressing appetite and boosting energy expenditure.
But in leptin resistance, despite elevated leptin levels—common in obesity—the brain misreads the signal, acting as if the body is starving. This results in increased hunger, reduced energy burn, and ongoing fat accumulation.
Recent research from Arizona State University has uncovered the role of a transcription factor known as Slug (also called Snai2) in driving leptin resistance.
This molecule appears to interfere with leptin signaling by modifying gene expression in key brain regions, particularly within leptin receptor–expressing neurons. By silencing leptin receptor genes, Slug effectively blocks the hormone’s satiety signal.
Beyond Slug, other epigenetic mechanisms are involved. These include DNA methylation of the leptin or leptin receptor genes, histone modifications, and microRNAs that inhibit leptin-related pathways. Interestingly, these changes may be long-lasting, contributing to persistent weight problems even after dieting or weight loss.
Studies also show that leptin receptors are present in the hippocampus, suggesting that leptin resistance may affect brain functions like memory and learning.
In cases of obesity, even after significant weight loss, the body can retain a kind of “epigenetic memory” that favors weight regain. This makes leptin resistance not just a hormonal issue, but a complex, multi-layered epigenetic condition that defies simple solutions.
Causes and Symptoms of Leptin Resistance
Leptin is a hormone produced by fat cells that helps regulate appetite and energy balance. It signals the brain to reduce hunger when fat stores are sufficient.
However, in individuals with leptin resistance, the brain fails to respond to leptin’s signals, leading to overeating and weight gain.
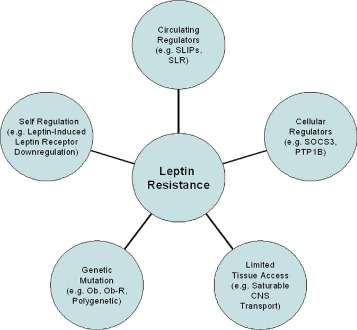
Several factors contribute to leptin resistance, each playing a significant role in disrupting this vital process.
Chronic Inflammation:
Inflammation in the hypothalamus—a critical brain region for regulating hunger—impairs leptin signaling.
According to research, individuals with leptin resistance often show elevated levels of inflammatory markers like C-reactive protein (CRP). Chronic low-grade inflammation weakens the brain’s sensitivity to leptin, causing persistent hunger signals even when fat stores are full.
Elevated Free Fatty Acids:
High levels of free fatty acids in the bloodstream can interfere with leptin’s ability to communicate with the brain.
As per scientific studies, excessive free fatty acids disrupt receptor function and reduce leptin transport across the blood-brain barrier, worsening resistance and promoting fat storage.
Genetic Predisposition:
Some individuals are genetically predisposed to leptin resistance.
Genetic variants associated with leptin or its receptor can impair normal signaling pathways, making these individuals more vulnerable to obesity despite lifestyle changes.
Common Symptoms:
The most noticeable symptoms of leptin resistance include constant hunger, especially cravings for high-calorie or sugary foods, difficulty losing weight despite efforts, and low energy levels.
Without proper management, leptin resistance can lead to metabolic disorders, insulin resistance, and increased risk of type 2 diabetes.
Addressing leptin resistance requires a multi-faceted approach, including reducing inflammation, managing blood sugar levels, and adopting a balanced diet rich in anti-inflammatory foods.
How Leptin Resistance Affects Weight Loss?
Leptin is a hormone secreted by fat cells that signals the brain to regulate appetite and energy expenditure. However, in leptin resistance—a condition common in obesity—the brain stops responding effectively to leptin’s signals, disrupting normal metabolic function.
Here’s how leptin resistance affects the body, according to top scientific studies:
Impaired Appetite Control:
In a leptin-resistant state, the brain fails to receive the “satiety” message, leading to a persistent sensation of hunger. Research published in Cell Metabolism shows that this miscommunication tricks the body into thinking it is starving, even when fat stores are excessive.
Increased Food Intake and Weight Gain:
Because the brain does not perceive enough leptin, it promotes compulsive eating and decreases voluntary physical activity. According to a review in Nature Reviews Endocrinology, this fosters a feedback loop of continued weight gain and worsening resistance.
Reduced Energy Expenditure:
Leptin normally encourages the body to burn energy when fat stores are high. With resistance, this signal weakens, and the body becomes more energy-conserving. As per findings in Diabetes Care, individuals with leptin resistance exhibit lower metabolic rates.
Insulin Resistance Link:
Leptin and insulin signaling pathways are closely linked. Studies from The Journal of Clinical Investigation demonstrate that leptin resistance often coexists with insulin resistance, compounding risks for Type 2 diabetes.
Inflammatory Feedback Loop:
Chronic inflammation, often seen in obesity, may further impair leptin signaling. Research in Endocrine Reviews suggests that inflammatory cytokines exacerbate leptin resistance, creating a metabolic storm.
Leptin resistance isn’t just a barrier to weight loss—it’s a deep-rooted hormonal disruption that fuels obesity, diabetes, and systemic inflammation.
Diagnosing Leptin Resistance
Diagnosing leptin resistance is not straightforward, as no single test can confirm the condition. However, several assessments can help provide a clearer picture:
Blood Leptin Level Measurement:
A common step in identifying leptin resistance is measuring leptin levels in the blood. High leptin levels, especially in individuals struggling with obesity and weight loss, may indicate leptin resistance. This suggests that although leptin levels are high, the brain is not responding to its signals to reduce hunger. As per the Cleveland Clinic, elevated leptin levels are often associated with disrupted appetite regulation in such cases.
Comprehensive Metabolic Panel:
Healthcare providers may recommend a comprehensive metabolic panel, which assesses blood sugar levels, liver and kidney function, and lipid profiles. According to the Mayo Clinic, abnormalities in these areas can indicate metabolic syndrome—a condition commonly linked to leptin resistance and obesity.
Inflammatory Marker Assessment:
Chronic inflammation is a known contributor to leptin resistance. Testing for inflammatory markers such as C-reactive protein (CRP) can help detect underlying inflammation. As per Healthline, high levels of CRP are frequently seen in individuals with metabolic disorders and leptin resistance.
While these tests provide important insights, they are not definitive. A thorough evaluation by healthcare providers, considering both clinical symptoms and test results, is crucial for diagnosing and managing leptin resistance effectively.
Effective Strategies to Manage Leptin Resistance
Managing leptin resistance requires a multifaceted approach, including dietary changes, lifestyle modifications, and sometimes medical intervention:
Leptin Resistance Diet
A diet focused on reducing inflammation and improving leptin sensitivity is crucial.
Incorporating “high leptin food” such as lean proteins, fibrous vegetables, and healthy fats can help manage hunger and improve leptin signaling.
Reducing intake of processed foods, refined sugars, and trans fats is also essential.
Leptin Resistance Supplements
Supplements like omega-3 fatty acids, turmeric, and green tea extract can reduce inflammation and support leptin sensitivity.
However, more research is needed to establish their effectiveness as a “leptin resistance treatment.”
Exercise and Physical Activity
Regular physical activity can help “improve leptin sensitivity” by reducing inflammation and enhancing the brain’s responsiveness to leptin signals.
Incorporating both aerobic and resistance training is beneficial for overall metabolic health.
Medical Interventions
In some cases, medications that target leptin signaling pathways or reduce inflammation may be prescribed to “fix leptin resistance.”
Research is ongoing to develop more targeted therapies that can “cure leptin resistance” and support sustainable weight loss.
FAQs On Leptin Resistance and Body Fat
Q-1: Why am I hungry even with high body fat—shouldn’t leptin be shutting hunger off?
A-1: In many people with excess fat, leptin levels are high but the “receiver” in the brain is dulled. Inflammation in hypothalamic circuits and signaling blockers (like SOCS proteins) muffle leptin’s message, so the brain keeps asking for food and defends a higher weight. Translation: your appetite isn’t a character flaw; it’s a throttled signal. Calmer inputs (better sleep, stress control, fewer ultra-processed foods) help the brain hear leptin again.
Q-2: Can ultra-processed foods make leptin resistance worse even at the same calories?
A-2: Yes. Soft textures, rapid eating, and low protein/fiber mean big bites with little stretch or chew—weak mechanical satiety. Add reward-heavy flavor layering and you eat faster before fullness hormones (including leptin’s partners) catch up. Practical fix: “slow the meal down” foods—crunchy veg, intact grains, and protein-first bites—plus a 10–15 minute pause before seconds.
Q-3: Why does dieting feel harder each week—am I losing willpower or losing leptin?
A-3: Dieting lowers leptin, and your brain treats that drop like a famine alarm: hunger rises, energy expenditure dips, and spontaneous movement (NEAT) shrinks. The trick isn’t to ignore biology but to outsmart it: use modest deficits, keep protein 1.6–2.2 g/kg, anchor fiber at ~10–15 g per 1,000 kcal, lift 2–3x/week to protect muscle, and schedule “maintenance” weeks to reset fatigue.
Q-4: Does circadian rhythm really change how leptin works?
A-4: Leptin follows a daily rhythm, peaking overnight to curb late snacking and support recovery. Late-night eating, shift work, or short sleep flatten that curve, blunting satiety and nudging cravings the next day. Quick wins: set a consistent wake time, front-load calories earlier, dim screens an hour pre-bed, and keep caffeine before noon. Many notice quieter late-night hunger within a week.
Q-5: What specifically improves leptin sensitivity—beyond “eat better, move more”?
A-5: Stack small levers:
- Meal design: protein-first, high-fiber sides, minimally processed carbs.
- Pace: 15-minute minimum mealtime, utensils down between bites.
- Activity: daily step floor (e.g., 7–10k) plus short post-meal walks to blunt glucose swings.
- Strength + intervals: lifts protect muscle (resting burn) and intervals enhance insulin/leptin signaling.
- Stress & sleep: 5-minute breathwork or a walk break mid-afternoon; 7–8 hours sleep.
These don’t “boost leptin” so much as remove static from the signal—making the same calories and workouts finally feel effective.
Can Leptin Resistance be Reversed – Conclusive Analysis
So, can leptin resistance be reversed?
The answer is yes, but it requires a comprehensive approach.
While there is no quick fix, adopting a healthy lifestyle, focusing on an anti-inflammatory diet, and incorporating regular exercise can significantly “reverse leptin resistance.”
Understanding the relationship between “leptin levels and obesity” is crucial for developing effective treatment plans.
For those struggling with weight loss, addressing leptin resistance might be the key to achieving sustainable results.
Consulting with healthcare professionals and considering a holistic approach can help “treatment of leptin resistance” and improve overall health and well-being.
References: