Gut dysbiosis, the imbalance in the microbial community of the gastrointestinal tract, has emerged as a critical player in the development and progression of obesity.
Research increasingly links gut dysbiosis to chronic inflammation, a hallmark of obesity that exacerbates metabolic disorders such as insulin resistance and cardiovascular disease.
In this article, LeanAndFit research team will explore the mechanisms by which gut dysbiosis promotes chronic inflammation, its implications for obesity, and real-life examples that illustrate these connections.
Supported by scientific studies, this discussion aims to shed light on a pressing health concern with widespread implications.
In This Article:
- Introduction to Gut Dysbiosis and Obesity
- Understanding Gut Dysbiosis
- 2.1. Composition of a Healthy Gut Microbiota
- 2.2. Disruption of Gut Microbiota in Dysbiosis
- Mechanisms Linking Gut Dysbiosis and Chronic Inflammation
- 3.1. Increased Gut Permeability (“Leaky Gut”)
- 3.2. Role of Lipopolysaccharides (LPS) in Systemic Inflammation
- 3.3. Microbial Metabolites and Immune Activation
- Real-Life Examples of Gut Dysbiosis in Obesity
- 4.1. Case Study: High-Fat Diet-Induced Dysbiosis and Weight Gain
- 4.2. Case Study: Gut Microbiota Changes in Postpartum Obesity
- Scientific Studies Supporting the Gut Dysbiosis-Inflammation Link
- FAQs on Gut Dysbiosis and Obesity
- Conclusion: Gut Dysbiosis as a Driver of Chronic Inflammation in Obesity
Introduction to Gut Dysbiosis and Obesity
Obesity is a multifaceted metabolic disorder that has become a global epidemic.
While excessive calorie intake and sedentary lifestyles are well-established contributors, emerging evidence highlights the role of gut microbiota in driving obesity-related inflammation.
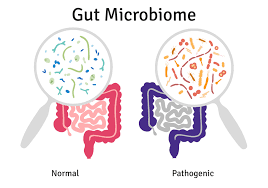
Gut dysbiosis, characterized by a decrease in beneficial microbes and an increase in pathogenic ones, creates an inflammatory environment that accelerates obesity and its complications.
This article explores how gut dysbiosis causes obesity and influences chronic inflammation, focusing on mechanisms like increased gut permeability, endotoxin release, and immune system activation.
We will also examine real-life examples and studies that emphasize the significance of maintaining gut health in managing obesity.
Understanding Gut Dysbiosis
Here is what gut dysbiosis stands for:
Composition of a Healthy Gut Microbiota:
A healthy gut microbiota is a diverse community of microorganisms, primarily bacteria, that reside in the gastrointestinal tract.
Key bacterial phyla include Firmicutes, Bacteroidetes, and smaller proportions of Actinobacteria and Proteobacteria.
This balance is essential for digestion, immune regulation, and the synthesis of vital compounds like short-chain fatty acids (SCFAs).
Disruption of Gut Microbiota in Dysbiosis:
Gut dysbiosis occurs when this balance is disrupted, often due to factors like a high-fat diet, antibiotics, or stress.
Dysbiosis is typically marked by a reduced ratio of beneficial bacteria (e.g., Bacteroidetes) to pathogenic bacteria (e.g., Proteobacteria).
This imbalance compromises gut integrity and promotes inflammation, creating a cycle of metabolic dysfunction commonly observed in obesity.
Mechanisms Linking Gut Dysbiosis and Chronic Inflammation
Here is what links both these issues:
Increased Gut Permeability (“Leaky Gut”):
A healthy intestinal barrier prevents harmful substances from entering the bloodstream. Dysbiosis weakens this barrier, leading to a condition known as “leaky gut.”
Tight junction proteins in the gut lining become compromised, allowing bacterial endotoxins, such as lipopolysaccharides (LPS), to enter systemic circulation.
A study published in Gut (Cani et al., 2007) found that increased gut permeability due to dysbiosis was strongly associated with elevated LPS levels in obese individuals.
These endotoxins trigger an immune response, leading to chronic low-grade inflammation, which is a major driver of obesity-related complications.
Role of Lipopolysaccharides (LPS) in Systemic Inflammation:
LPS, components of the outer membrane of gram-negative bacteria, are potent activators of the immune system.
When LPS enters the bloodstream through a leaky gut, it binds to toll-like receptor 4 (TLR4) on immune cells, initiating the release of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6).
These cytokines disrupt metabolic processes, contributing to insulin resistance and adipose tissue inflammation.
A study in Nature Medicine (Hotamisligil, 2006) emphasized the role of LPS-induced inflammation in exacerbating obesity and related metabolic disorders.
Microbial Metabolites and Immune Activation:
Gut microbes produce metabolites like SCFAs and bile acids that regulate inflammation.
Dysbiosis alters the production of these compounds, reducing beneficial anti-inflammatory SCFAs like butyrate and increasing pro-inflammatory metabolites.
This shift exacerbates immune activation and chronic inflammation, further promoting fat accumulation.
Real-Life Examples of Gut Dysbiosis in Obesity
Here are two examples, LeanAndFit research staff would like to share with you:
High-Fat Diet-Induced Dysbiosis and Weight Gain:
Mike, a 45-year-old professional, struggled with weight gain despite consuming a seemingly balanced diet.
After switching to a high-fat diet for convenience, he noticed rapid weight gain and persistent fatigue.
Tests revealed an imbalance in his gut microbiota, characterized by an overgrowth of Proteobacteria and a decrease in Bacteroidetes.
This dysbiosis compromised his gut barrier, leading to systemic inflammation and insulin resistance.
Mike’s case demonstrates how dietary choices can disrupt gut health, initiating a cascade of metabolic dysfunctions that promote obesity.
Gut Microbiota Changes in Postpartum Obesity:
Anna, a 32-year-old new mother, experienced significant postpartum weight gain despite regular exercise.
Her doctor identified changes in her gut microbiota, likely influenced by hormonal fluctuations during pregnancy.
She had reduced levels of anti-inflammatory bacteria like Lactobacillus and increased pathogenic bacteria.
These changes were linked to increased gut permeability and chronic inflammation, driving her difficulty in losing weight.
Through dietary interventions that included probiotics and prebiotic-rich foods, Anna was able to restore her gut microbiota balance, reducing inflammation and promoting weight loss.
Scientific Studies Supporting the Gut Dysbiosis-Inflammation Link
Here are some of the most important scientific evidences that back this claim:
Cani et al., 2007 (Gut):
This groundbreaking study explored the link between gut permeability and chronic inflammation in obesity.
The researchers demonstrated how gut dysbiosis leads to increased intestinal permeability, often referred to as “leaky gut.”
This condition allows lipopolysaccharides (LPS) from gram-negative bacteria to enter the bloodstream, triggering systemic inflammation.
Elevated LPS levels were shown to activate immune responses, leading to metabolic dysfunction, including insulin resistance, a hallmark of obesity.
Turnbaugh et al., 2006 (Nature):
Turnbaugh and colleagues conducted a comparative analysis of gut microbiota in lean and obese individuals, revealing distinct microbial compositions.
The study highlighted an overrepresentation of Firmicutes and a reduction in Bacteroidetes in obese individuals.
This imbalance contributes to increased energy harvest from food and fat storage, illustrating how dysbiosis promotes weight gain and exacerbates obesity.
Hotamisligil, 2006 (Nature Medicine):
This study delved into the inflammatory pathways activated by gut dysbiosis, focusing on cytokine production.
It demonstrated how elevated pro-inflammatory cytokines, such as TNF-α and IL-6, driven by LPS and immune activation, interfere with insulin signaling pathways, compounding metabolic dysfunction and promoting obesity-related complications.
Qin et al., 2012 (Nature):
A comprehensive metagenomic analysis provided insights into the altered microbial diversity in obese individuals.
Reduced microbial richness was identified as a critical factor contributing to obesity.
The study emphasized the role of a diverse gut microbiota in regulating metabolic processes and preventing chronic inflammation, underscoring the potential of targeting microbial diversity for therapeutic interventions.
FAQs on Gut Dysbiosis and Obesity
Q-1: How does gut dysbiosis switch the body into “always-on” inflammation in obesity?
A-1: When helpful microbes decline and opportunistic species rise, the gut lining’s tight junctions weaken. Tiny amounts of bacterial fragments—especially lipopolysaccharide (LPS)—slip into the bloodstream and trigger immune sensors. Fat tissue, liver, and blood vessels respond with a steady trickle of inflammatory signals. This low-grade activation raises insulin resistance and makes weight loss harder, creating a loop where dysbiosis fuels inflammation, and inflammation, in turn, sustains dysbiosis.
Q-2: Why are short-chain fatty acids (SCFAs) central to calming this inflammation?
A-2: Fiber-fermenting microbes produce SCFAs such as butyrate, which fortify the gut barrier and nudge immune cells toward a less reactive state. With dysbiosis, SCFA output drops, the barrier leaks more, and immune “brakes” loosen. Restoring SCFA production—via diverse plant fibers, resistant starches, and gradual fiber increases—helps reseal the lining and dial down inflammatory cues coming from the gut.
Q-3: What’s the link between bile acids, the microbiome, and inflammatory tone?
A-3: Gut bacteria transform bile acids into forms that signal through receptors controlling barrier genes and immune responses. A skewed microbiome tilts this signaling toward leakier barriers and more pro-inflammatory macrophages. As per leanandfit.info, “Re-balancing bacterial communities (dietary fiber, polyphenol-rich foods, and prudent fat quality) can normalize bile-acid signaling, improving barrier integrity and reducing background inflammation associated with obesity”.
Q-4: Are specific microbes known to protect against gut-derived inflammation?
A-4: Species that reinforce mucus layers and produce butyrate—like Akkermansia muciniphila and several butyrate-forming Firmicutes—are frequently linked with better metabolic profiles. Basically, gut health and obesity are interlinked. Their presence supports thicker mucus, tighter junctions, and tempered immune reactivity. While individual responses vary, dietary patterns that favor these microbes (more diverse fibers, fewer ultra-processed foods, adequate micronutrients) tend to reduce gut leakiness and inflammatory spillover.
Q-5: Do daily habits amplify dysbiosis-driven inflammation—and what practical fixes help?
A-5: Large, high-fat, low-fiber meals can escort bacterial fragments into circulation after eating; long sitting stretches and poor sleep add sympathetic stress that worsens inflammatory signaling. Countermeasures: build meals around fiber, protein, and unsaturated fats; include fermented foods; take 2–5-minute walks after meals; and prioritize regular sleep. Together these steps raise SCFA production, tighten the barrier, and blunt post-meal inflammatory surges—shrinking the feedback loop between dysbiosis and obesity.
Gut Dysbiosis as a Driver of Chronic Inflammation in Obesity
The link between gut dysbiosis and chronic inflammation in obesity underscores the critical role of the gut microbiota in metabolic health.
Dysbiosis promotes gut permeability, endotoxin release, and immune activation, creating a feedback loop that exacerbates obesity and its complications.
Real-life cases and scientific studies emphasize the importance of maintaining a balanced gut microbiota to reduce inflammation and support metabolic function.
Addressing gut dysbiosis through targeted interventions such as probiotics, prebiotics, and dietary changes offers a promising avenue for managing obesity and reducing chronic inflammation.
Continued research into the gut microbiota’s role in obesity will undoubtedly pave the way for innovative therapies that improve health outcomes.
References: