Excess body fat is a significant contributor to various health conditions, with arterial stiffness being one of the most concerning.
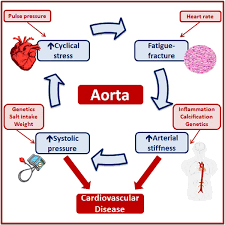
Arterial stiffness refers to the reduced elasticity of the arteries, which affects their ability to expand and contract in response to blood flow.
This condition is closely associated with cardiovascular diseases, hypertension, and metabolic disorders.
In this article, we will explore how excess body fat contributes to arterial stiffness, including its underlying mechanisms, symptoms, and methods for assessment.
By understanding this link, we can gain valuable insights into mitigating the risks of arterial stiffness.
In This Article:
- Understanding Arterial Stiffness
- The Role of Excess Body Fat in Arterial Stiffness
- Impact of Visceral Fat on Arterial Health
- Inflammatory Pathways and Arterial Stiffness
- Insulin Resistance and Endothelial Dysfunction
- Arterial Stiffness Symptoms and Indicators
- How to Measure and Assess Arterial Stiffness
- FAQs on Excess Body Fat & Arterial Stiffness
- Real-Life Example: John’s Journey
- Conclusion: The Critical Link Between Body Fat and Arterial Health
Understanding Arterial Stiffness
Arterial stiffness refers to the reduced elasticity of arterial walls, impairing their ability to expand and contract in response to blood flow.
In healthy arteries, this elasticity helps maintain optimal blood flow and consistent blood pressure levels.
However, stiffened arteries become less compliant, causing increased resistance to blood flow and elevating systolic blood pressure.
Over time, this can place significant strain on the cardiovascular system, increasing the heart’s workload and leading to long-term health complications.
What Does Arterial Stiffness Indicate?
Arterial stiffness is more than a symptom of aging—it is a critical predictor of cardiovascular health. It often signals the onset of conditions such as hypertension, stroke, and heart failure.
A study published in the Journal of Hypertension (2021) highlighted arterial stiffness as a biomarker of vascular aging, noting its strong association with cardiovascular morbidity and mortality.
Recognizing and understanding this condition is essential for identifying underlying risk factors and preventing long-term cardiovascular disease.
By evaluating arterial stiffness, clinicians can gain insights into a patient’s vascular health, enabling targeted interventions that address root causes, such as excess body fat and lifestyle-related factors.
This proactive approach is vital for mitigating its impact on cardiovascular health.
The Role of Excess Body Fat in Arterial Stiffness
Excess body fat contributes to arterial stiffness through various mechanisms, including direct physical effects, hormonal imbalances, and chronic inflammation.
Impact of Visceral Fat on Arterial Health:
Visceral fat, stored around internal organs, plays a critical role in arterial stiffness. Unlike subcutaneous fat, visceral fat is metabolically active, releasing free fatty acids and hormones that influence arterial function.
- Association Between Body Fat Parameters and Arterial Stiffness: A study published in Obesity Reviews (2019) highlighted a direct correlation between increased visceral fat and arterial stiffness, showing that higher waist circumference and body fat percentage were strongly associated with reduced arterial elasticity.
Inflammatory Pathways and Arterial Stiffness:
Excess body fat triggers chronic low-grade inflammation, a major contributor to arterial stiffness. Adipose tissue releases pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), which damage arterial walls and reduce elasticity.
- Mechanism: These inflammatory mediators impair the production of nitric oxide, a molecule critical for vascular relaxation, leading to endothelial dysfunction.
Insulin Resistance and Endothelial Dysfunction:
Excess body fat often leads to insulin resistance, which has a direct impact on arterial stiffness. Insulin resistance reduces the bioavailability of nitric oxide and promotes vascular inflammation.
- Study Insight: A study in Diabetes Care (2020) found that individuals with central obesity and insulin resistance exhibited higher arterial stiffness compared to those with normal glucose tolerance.
Arterial Stiffness Symptoms and Indicators
Arterial stiffness often progresses silently, making early detection challenging. However, certain symptoms and physical indicators may suggest its presence:
- Elevated Systolic Blood Pressure: Stiff arteries lead to increased systolic blood pressure, as the heart must pump harder to circulate blood through less elastic vessels.
- Reduced Physical Endurance: Individuals may feel fatigued or have difficulty performing physical activities due to compromised blood flow.
- Shortness of Breath During Exertion: Restricted arterial function affects oxygen delivery, making exertion physically taxing.
- Leg Cramps or Discomfort: Poor blood circulation due to arterial stiffness can result in muscle cramping or discomfort, particularly in the legs.
What Contributes to Arterial Stiffness?
Several factors can amplify the effects of excess body fat on arterial stiffness, including:
- Age: Arterial elasticity naturally diminishes with age. When combined with obesity, this process accelerates significantly.
- Hypertension: Elevated blood pressure, often associated with obesity, places additional stress on arterial walls, leading to stiffening.
- Poor Diet: Diets rich in saturated fats, sugars, and processed foods contribute to fat accumulation, oxidative stress, and vascular inflammation.
These factors often work synergistically, highlighting the importance of lifestyle changes to mitigate arterial stiffening.
How to Measure and Assess Arterial Stiffness?
Accurately assessing arterial stiffness is critical for understanding cardiovascular health and taking preventive measures.
Advances in technology provide reliable methods to measure and evaluate arterial stiffness.
How to Measure Arterial Stiffness?
- Pulse Wave Velocity (PWV)
Considered the gold-standard method, PWV calculates the speed at which blood pressure waves propagate through the arterial system. Stiffer arteries result in faster wave velocities. PWV is non-invasive and provides crucial insights into vascular health. A study in Hypertension Research (2020) noted that increased PWV correlates with cardiovascular risk factors such as obesity and hypertension. - Augmentation Index (AIx)
This method examines pressure waveforms to evaluate arterial stiffness and wave reflection. AIx is particularly useful in assessing how arterial stiffness impacts systolic blood pressure, offering predictive insights into cardiovascular health.
How Do You Assess Arterial Stiffness?
Evaluating arterial stiffness typically involves combining these measurement techniques with clinical assessments. Healthcare providers often include:
- Blood Pressure Monitoring to track hypertension, a major contributor to arterial stiffness.
- Imaging Tools, such as ultrasound, to visualize arterial structure and identify abnormalities.
By integrating these methods, medical professionals can detect arterial stiffness early, paving the way for targeted interventions to mitigate cardiovascular risks.
FAQs on Excess Body Fat & Arterial Stiffness
Q-1: What’s the first domino—how does excess body fat start making arteries stiffer?
A-1: Central (visceral) fat bathes the liver and vessels in free fatty acids and inflammatory signals. Endothelial cells lose nitric oxide, the vessel’s natural “relax” chemical, and smooth muscle tone creeps upward. Over time, the wall remodels—more collagen, less elastic fiber function—so each heartbeat meets a “stiffer pipe,” raising pulse pressure.
Q-2: Is it just inflammation, or do hormones from fat also harden arteries?
A-2: Hormones shift too. Adiponectin (vessel-protective) tends to fall, while leptin and angiotensin activity rise, nudging sympathetic tone and sodium retention upward. The combined effect elevates resting vascular tone and encourages fibrosis in the arterial wall—two hallmarks of greater arterial stiffness.
Q-3: Why does belly fat specifically matter more than weight elsewhere?
A-3: Visceral depots sit close to major vessels and the portal vein, so their signals reach the liver and arteries quickly and in high concentration. Perivascular adipose tissue—fat wrapped around arteries—also changes character with obesity, releasing fewer relaxing factors and more pro-contractile ones. That local “neighborhood effect” accelerates stiffening compared with fat stored in hips or limbs.
Q-4: Can high blood sugar from insulin resistance stiffen arteries even before diabetes is diagnosed?
A-4: Yes. Repeated post-meal spikes promote advanced glycation of vessel proteins and oxidative stress, which cross-link collagen and impair elastin. You may still have “normal” fasting glucose while pulse pressure widens and pulse wave velocity creeps up—early signs that metabolic strain is already degrading arterial springiness.
Q-5: What practical signs and steps point to fat-related arterial stiffness—and how do you reverse it?
A-5: Clues include a rising waist-to-height ratio (>0.5), widening pulse pressure, and “normal” clinic BP that masks higher home or nighttime values. Reversal targets the drivers: trim visceral fat with a modest calorie deficit; prioritize protein and fiber; add resistance training plus 150–300 minutes/week of aerobic work; walk 10–15 minutes after meals to blunt glucose spikes; sleep 7–9 hours to normalize sympathetic tone. Even a 5–10% weight reduction can lower arterial stiffness measures, while blood-pressure control and reduced sodium help the vessel wall recover.
Takeaway: Excess—and especially abdominal—fat stiffens arteries via endothelial dysfunction, hormonal shifts, and structural remodeling of the vessel wall. Catch it early with waist-centric and hemodynamic clues, then chip away at visceral fat and sympathetic load to restore arterial flexibility.
John’s Journey: A Real-Life Example of Arterial Stiffness and Obesity
Excess body fat and its contribution to arterial stiffness are more than just clinical terms; they affect real lives.
John’s experience exemplifies how lifestyle factors and interventions can profoundly impact arterial health.
Background: The Struggle with Obesity
John, a 45-year-old office worker, led a sedentary lifestyle characterized by long hours at a desk, frequent consumption of processed foods, and limited physical activity.
Over a decade, his weight steadily increased, culminating in a body mass index (BMI) of 32, classifying him as obese.
John frequently experienced fatigue, high blood pressure, and chest discomfort, but he attributed these symptoms to stress and aging.
Diagnosis: Identifying the Root Cause
Concerned about his symptoms, John visited a cardiologist.
A series of tests, including pulse wave velocity (PWV) to measure arterial stiffness, revealed significant stiffening in his arteries—a hallmark of cardiovascular strain.
Additional evaluations highlighted elevated visceral fat, high systolic blood pressure, and markers of systemic inflammation, such as C-reactive protein (CRP).
The diagnosis pointed to obesity as a primary contributor to his arterial stiffness.
Intervention: Taking Action
Motivated by his diagnosis, John embarked on a structured weight-loss plan under medical supervision.
He adopted a balanced diet rich in fruits, vegetables, lean proteins, and whole grains while reducing his intake of saturated fats and sugars.
John also committed to 30 minutes of daily aerobic exercise, such as brisk walking and cycling. He also opted for healthy snacks while travelling.
Over six months, he reduced his visceral fat by 15%, leading to improved PWV measurements and a noticeable decrease in blood pressure.
Outcome: Lessons from John’s Journey
John’s symptoms of fatigue and chest discomfort diminished as his arterial stiffness decreased.
This case highlights the significant relationship between excess body fat and arterial health while demonstrating that lifestyle changes can reverse or mitigate arterial stiffness.
His story serves as a reminder of the importance of early diagnosis and proactive intervention in managing obesity-related cardiovascular risks.
John’s journey underscores that arterial stiffness, though serious, can be addressed through sustained lifestyle adjustments and guided meditation to reduce extra bodyfat.
By reducing excess body fat, individuals can improve their cardiovascular health and overall quality of life.
The Critical Link Between Body Fat and Arterial Health
Excess body fat plays a critical role in the development of arterial stiffness by triggering inflammation, disrupting insulin sensitivity, and causing hormonal imbalances.
As per leanandfit.info, “Visceral fat, in particular, releases pro-inflammatory cytokines like IL-6 and TNF-α, which damage arterial walls and reduce elasticity”.
Insulin resistance, often associated with obesity, contributes further by impairing vascular endothelial function and exacerbating stiffness.
Additionally, adipokines such as leptin and adiponectin, which regulate vascular health, become imbalanced in individuals with excess body fat.
Early detection is key to mitigating the risks associated with arterial stiffness.
Non-invasive tools like Pulse Wave Velocity (PWV) are commonly used to measure arterial stiffness, providing valuable insights into vascular health.
Interventions targeting body fat reduction, including dietary changes, exercise, and lifestyle adjustments, can significantly improve arterial flexibility and reduce cardiovascular risks.
Understanding the association between body fat parameters and arterial stiffness empowers individuals and healthcare providers to address these underlying causes effectively.
This proactive approach is crucial for enhancing vascular function, minimizing complications like hypertension and heart disease, and promoting overall well-being.
The growing body of research underscores the importance of managing body fat to protect arterial health and ensure long-term cardiovascular resilience.
References: