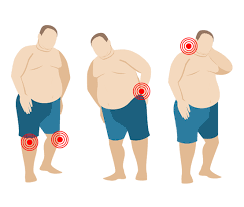
Joint pain and obesity often coexist, forming a cycle that is challenging to break.
Joint pain limits mobility, while reduced physical activity leads to weight gain, exacerbating the strain on joints.
In this article, LeanAndFit will explore the intricate relationship between joint pain and obesity, examining how and why these conditions are interconnected.
We will discuss the impact of reduced physical activity due to joint pain, metabolic changes caused by inflammation, and the psychological components that further complicate weight management.
Real-life examples will highlight these issues, making the discussion relatable and practical.
Finally, the role of specific joints and their vulnerability to weight-related pain will be analyzed, backed by scientific studies.
Article Index
- Introduction: The Cycle of Joint Pain and Obesity
- How Joint Pain Limits Physical Activity
- Metabolic Changes Linking Pain and Weight Gain
- Psychological Stress: A Catalyst for Obesity
- Specific Joint Conditions and Weight Gain
- Knee Pain and Daily Living
- Sacroiliac Joint Pain and Its Role in Obesity
- Real-Life Examples of Joint Pain Leading to Obesity
- Conclusion
The Cycle of Joint Pain and Obesity
Joint pain and obesity are closely intertwined, creating a self-perpetuating cycle that is challenging to break.
Chronic joint pain, especially in weight-bearing areas like the knees, hips, and lower back, often discourages physical activity.
Reduced mobility (such as sitting in your office chair) leads to a decline in calorie expenditure, promoting gradual fat accumulation.
As weight increases, the added stress on joints worsens pain, further limiting physical activity and perpetuating the cycle.
For instance, each additional pound of body weight adds roughly four pounds of pressure on the knees, accelerating cartilage wear and increasing pain.
This pain not only impairs physical health but also impacts mental well-being, leading to stress, anxiety owing to body image issues, and even depression.
These psychological factors can encourage unhealthy coping mechanisms, such as overeating, compounding the problem.
Addressing this cycle requires a holistic approach, including weight management, physical therapy, and psychological support, to improve joint function, reduce pain, and restore overall health and mobility.

How Joint Pain Limits Physical Activity?
Joint pain, particularly in weight-bearing areas like the knees, hips, and lower back, significantly impacts mobility and limits physical activity.
The discomfort or sharp pain experienced during movement makes even basic tasks difficult, leading individuals to avoid activities that strain their joints.
This avoidance can lead to a sedentary lifestyle, which further exacerbates weight gain and decreases overall fitness levels.
For example, knee pain often hinders activities of daily living such as walking, climbing stairs, or standing for extended periods. Individuals with chronic knee pain may find it challenging to exercise, take leisurely walks, or engage in recreational activities, further reducing their energy expenditure.
Similarly, hip pain can interfere with bending, sitting, or even sleeping comfortably, leading to a decline in overall physical function.
Research underscores the impact of joint pain on activity levels.
A 2017 study published in Arthritis Care & Research found that people with chronic joint pain were 35% less active than those without pain, demonstrating how pain-induced inactivity is a major contributor to weight gain.
The combination of reduced movement and metabolic changes from chronic pain creates a vicious cycle, where weight gain worsens joint stress, intensifying pain and further limiting activity.
Addressing joint pain through physical therapy, low-impact exercises, and weight management is critical to breaking this cycle and restoring mobility.
Metabolic Changes Linking Pain and Weight Gain
Chronic joint pain frequently coexists with inflammation, a biological response that significantly impacts the body’s metabolism.
Inflammation triggers hormonal imbalances, particularly elevated cortisol levels, which promote fat storage and weight gain.
This metabolic shift creates a cycle where pain worsens inflammation, and inflammation further impairs the body’s ability to regulate weight.
The link between pain, inflammation, and weight gain is well-documented.
Conditions like arthritis, which are characterized by chronic inflammation, not only intensify pain but also disrupt metabolic processes, making weight loss challenging.
Inflammatory cytokines—proteins released during inflammation—can impair insulin sensitivity, leading to increased fat accumulation and a higher risk of obesity.
A study published in The Journal of Endocrinology highlights this relationship, emphasizing how chronic inflammation affects insulin regulation and fat metabolism.
Addressing both inflammation and joint pain is crucial for breaking this cycle and restoring metabolic balance, thereby improving overall health.
Psychological Stress: A Catalyst for Obesity
Chronic joint pain not only affects physical health but also has a profound impact on mental well-being. Individuals living with persistent joint pain often experience emotional stress, anxiety, and depression.
These psychological challenges can trigger unhealthy coping mechanisms, such as overeating, especially foods high in sugar and fat that provide temporary emotional relief.
This cycle of stress-induced eating contributes significantly to weight gain, complicating the management of both joint pain and obesity.
The connection between joint pain, mental health, and obesity extends beyond physical limitations.
Struggling with chronic pain often leads to feelings of frustration, helplessness, and low self-esteem, which can make adopting healthier habits feel overwhelming.
The emotional toll can create a self-perpetuating cycle: joint pain leads to stress, stress encourages overeating, and weight gain further worsens joint pain.
Research supports this relationship.
A study published in Psychosomatic Medicine revealed that individuals with chronic pain were 50% more likely to develop stress-related eating habits compared to those without pain.
This highlights how psychological factors amplify the challenge of weight management.
Breaking this cycle requires a multidisciplinary approach that addresses not only the physical symptoms of joint pain but also the mental and emotional barriers to healthier living.
Specific Joint Conditions and Weight Gain
Here are 2 such cases that I can think about:
Knee Pain and Daily Living:
The knee is one of the most vulnerable joints to weight-related pain, as excess body weight places immense stress on this critical load-bearing joint.
Each pound of extra body weight translates to four pounds of additional pressure on the knees during walking, leading to accelerated cartilage wear and a heightened risk of osteoarthritis.
Over time, this strain can result in chronic knee pain, severely affecting mobility and daily activities.
The impact on joint health is significant. Research shows that individuals with knee pain often experience a 20–30% reduction in mobility, as reported in the American Journal of Sports Medicine.
This decreased activity creates a cycle where limited movement contributes to weight gain, which, in turn, worsens joint pain.
Such compounding factors make addressing knee pain essential for maintaining both physical and overall health.
Sacroiliac Joint Pain and Its Role in Obesity:
The sacroiliac (SI) joint, which connects the spine to the pelvis, is another joint significantly affected by obesity.
This joint plays a crucial role in weight-bearing activities like standing, walking, and bending.
Pain in the SI joint often leads to reduced physical activity, which contributes to weight gain and fat accumulation.
The increased weight further exacerbates SI joint dysfunction, creating a cycle of pain and immobility.
A 2020 study published in Pain Medicine found that obesity increases the prevalence of SI joint dysfunction by 25%.
This highlights the interconnected nature of weight, joint health, and mobility, underscoring the need for a comprehensive approach to prevention and management.
Case Study: Jane’s Struggle with Weight and Joint Pain
Jane, a 45-year-old teacher, faced a challenging health journey after sustaining a knee injury.
Initially active and energetic, the injury significantly limited her mobility, causing her to struggle with day-to-day activities. Over time, the persistent joint pain in her knee spread to her hips and lower back, making movement increasingly difficult.
Unable to engage in her usual physical activities, Jane turned to food for comfort, developing stress-induced eating habits. Within a year, she gained 30 pounds, which further aggravated her joint pain and mobility issues.
This additional weight created a vicious cycle: the more she gained, the more stress her joints endured, intensifying her pain and making exercise even more daunting.
Jane consulted a physical therapist who explained how the combination of inactivity and weight gain exacerbated her condition. Through therapy, Jane started small, incorporating gentle bodyweight exercises to rebuild strength and reduce stress on her joints.
Her story illustrates the interconnected nature of joint pain and obesity.
Chronic pain limits activity, leading to weight gain, which further worsens joint issues.
Breaking this cycle requires a multidisciplinary approach, combining physical rehabilitation, dietary adjustments, and psychological support to address both the physical and emotional toll of these conditions.
Conclusion
Joint pain and obesity are deeply interconnected, forming a cycle that is challenging to break.
The combination of reduced mobility, metabolic changes, and psychological stress creates a scenario where weight gain worsens joint pain, further limiting physical activity.
Understanding this relationship is crucial for early intervention and targeted management strategies.
References: