It is no secret that abdominal fat is the bane of many people’s existence.
But did you know that it is more than just a cosmetic concern?
Beyond squeezing into your favorite pair of jeans, abdominal fat plays a significant role in health, particularly when it comes to triggering type 2 diabetes.
In this article, LeanAndFit shall delve into the intricate relationship between abdominal fat and type 2 diabetes, explain the science behind it, and offer practical solutions to keep both at bay.
Article Index:
- What is Abdominal Fat and Why Does it Matter?
- The Connection Between Visceral Fat and Type 2 Diabetes
- How Abdominal Fat Affects Insulin Resistance
- The Role of Inflammation in Diabetes Development
- Real-Life Example: Sarah’s Struggle with Belly Fat and Diabetes
- How to Combat Abdominal Fat to Prevent Type 2 Diabetes
- FAQs on Abdominal Fat in Triggering Type 2 Diabetes
- Conclusion: A Path to a Healthier Future
What is Abdominal Fat and Why Does it Matter?
Abdominal fat is not just about a few extra inches around your waistline.
It comes in two main types: subcutaneous fat, which lies just beneath the skin, and visceral fat, which wraps around internal organs like the liver, pancreas, and intestines.
Visceral fat is the real troublemaker here.
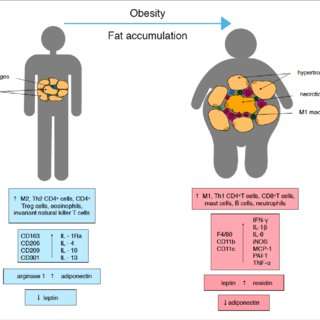
Unlike subcutaneous fat, visceral fat is metabolically active and releases fatty acids, hormones, and inflammatory markers into your bloodstream.
These substances disrupt metabolic processes, increasing your risk for conditions like type 2 diabetes mellitus.
A study published in Diabetes Care (2019) found that individuals with high levels of visceral fat were nearly twice as likely to develop type 2 diabetes compared to those with less belly fat.
What’s the Link?
Visceral fat is not just an innocent bystander—it is an active disruptor.
Unlike subcutaneous fat (the pinchable stuff just beneath your skin), visceral fat wraps itself around your organs and acts like a hormonal factory gone haywire.
It churns out cytokines, such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-6, which are inflammatory substances that wreak havoc on your body’s insulin signaling pathways.
When these pathways are compromised, insulin struggles to do its job of moving glucose into cells for energy.
This results in higher blood sugar levels and greater insulin resistance.
Scientific Backing
Research published in the Journal of Endocrinology and Metabolism (2020) confirmed the strong link between visceral fat and type 2 diabetes.
The study revealed that individuals with higher levels of visceral fat exhibited significantly reduced insulin sensitivity.
This fat type forces the pancreas to produce more and more insulin to regulate blood sugar, eventually leading to pancreatic burnout and full-blown diabetes.
Why It is Dangerous?
Think of visceral fat as a rogue tenant in your body—it does not just squat there; it actively creates chaos.
By releasing harmful inflammatory markers and disrupting your body’s glucose management system, it paves the way for chronic conditions like type 2 diabetes.
It also increases the risk of other metabolic issues, including heart disease and liver dysfunction.
The takeaway?
Reducing visceral fat is not just about aesthetics; it is a critical step in preventing type 2 diabetes and safeguarding your overall health.
How Abdominal Fat Affects Insulin Resistance?
Let me walk you through these simple yet trivial aspects that link fat with diabetes.
What is Insulin Resistance?
Insulin is your body’s key to unlocking energy.
It allows glucose (sugar) from your bloodstream to enter cells, where it is used for energy or stored for later.
But when you carry excess belly fat, particularly visceral fat, this process starts to falter.
Your cells become less responsive to insulin, a condition called insulin resistance.
To compensate, your pancreas shifts into overdrive, producing more insulin to manage blood sugar levels.
Over time, this chronic demand exhausts the pancreas, paving the way for type 2 diabetes.
The Science:
A pivotal study published in The Lancet (2018) demonstrated the connection between abdominal fat and insulin resistance.
Participants with high visceral fat levels had drastically reduced insulin sensitivity, making glucose regulation a constant battle for their bodies.
This study cemented the idea that belly fat isn’t just a cosmetic concern—it is a metabolic disruptor.
Real-Life Impact
Imagine trying to fit a square peg into a round hole—that is what happens when insulin cannot properly “unlock” your cells.
Belly fat creates this disconnect by releasing inflammatory markers and disrupting hormone signals, leaving glucose trapped in your bloodstream.
This not only raises your blood sugar levels but also leaves your cells deprived of the energy they need.
Over time, this imbalance triggers a cascade of metabolic issues, leading to type 2 diabetes and other chronic health conditions.
The takeaway? Reducing belly fat is key to restoring insulin sensitivity and improving overall metabolic health.
The Role of Inflammation in Diabetes Development
Visceral fat does not just disrupt insulin—it also fans the flames of chronic inflammation.
Inflammation is your body’s natural response to injury, but when it becomes chronic (as in the case of excess abdominal fat), it wreaks havoc on your metabolic system.
How Inflammation Works?
Inflammatory markers released by visceral fat interfere with insulin signaling pathways, worsening insulin resistance.
Chronic inflammation also damages beta cells in the pancreas, which produce insulin, leading to the progression of type 2 diabetes.
The Research
A study from Nature Medicine (2020) highlighted how belly fat and type 2 diabetes are connected through inflammatory pathways.
The study found that higher levels of C-reactive protein (an inflammation marker) correlated with increased diabetes risk.
Tom’s Battle with Belly Fat and Diabetes
Meet Tom, a 45-year-old software developer who loved late-night snacks and long hours in front of his computer.
Over time, his active college days became a distant memory, and his waistline expanded into a noticeable bulge.
At a routine check-up, his doctor flagged elevated blood sugar levels and warned him he was on the verge of developing type 2 diabetes.
The culprit? Excess abdominal fat.
Feeling alarmed but motivated, Tom decided to make changes.
He started with brisk 15-minute walks around his neighborhood every evening.
Recognizing the role of diet, he swapped his daily soda for water and introduced more fiber-rich foods like oatmeal and leafy greens into his meals.
Gradually, he added strength training to his routine and cut back on processed snacks.
Six months later, Tom had shed 12 pounds of belly fat.
His blood sugar levels were back within the normal range, and he felt more energized than he had in years.
Beyond the numbers, Tom experienced a renewed sense of confidence and control over his health.
Tom’s journey underscores the power of small, consistent changes.
With determination and practical adjustments, he reversed his prediabetes and proved that abdominal fat does not have to dictate your health outcomes.
How to Combat Abdominal Fat to Prevent Type 2 Diabetes?
Now that we have scared you (just a little) about the dangers of abdominal fat, let’s talk solutions.
>>> Adopt a Balanced Diet:
Focus on whole, unprocessed foods. Avoid sugary drinks, refined carbs, and trans fats—all of which contribute to visceral fat. A diet rich in lean protein, vegetables, and healthy fats can help you shed belly fat and improve insulin sensitivity.
Pro Tip:
Foods with a low glycemic index (like oats and lentils) are great for stabilizing blood sugar levels.
>>> Stay Active:
Physical activity is your best weapon against belly fat. Aim for a mix of cardio and strength training to maximize fat loss and improve insulin sensitivity.
Example Workout:
Try 30 minutes of brisk walking combined with 15 minutes of bodyweight exercises like squats and planks.
>>> Get Enough Sleep:
Lack of sleep can disrupt hormones that regulate hunger and fat storage, making it harder to lose belly fat. Aim for 7-9 hours of quality sleep each night.
>>> Manage Stress:
Chronic stress triggers cortisol production, which encourages fat storage in the abdominal region.
Incorporate stress-relief techniques like yoga, meditation, or deep breathing into your daily routine.
>>> Regular Check-Ups:
Do not skip your annual physical.
Regular screenings can catch early signs of insulin resistance, helping you address the issue before it escalates into type 2 diabetes.
Does Obesity Cause Diabetes or Does Diabetes Cause Obesity?
Ah, the age-old conundrum: what came first—the extra weight or the blood sugar spike?
Obesity, particularly visceral fat (that pesky fat around your organs), is like the annoying coworker who makes everyone’s job harder.
It fuels insulin resistance and ramps up inflammation, paving the way for type 2 diabetes.
But diabetes isn’t exactly an innocent bystander either—it strikes back by promoting weight gain.
How?
Elevated insulin levels, a hallmark of diabetes management, can turn your body into a fat-storing machine, particularly in the abdominal region.
The relationship is a toxic love story: obesity and diabetes enabling each other in a vicious cycle of health woes.
The solution? A holistic breakup.
Target the root causes—poor diet, lack of exercise, and stress—and simultaneously address the symptoms.
Think balanced meals, daily movement, and realistic goals. Who says you can’t ditch a toxic relationship and thrive?
FAQs on Abdominal Fat in Triggering Type 2 Diabetes
Q-1: Why does belly (visceral) fat raise diabetes risk more than weight carried on the hips or thighs?
A-1: Visceral fat drains into the portal vein, sending a steady stream of fatty acids and inflammatory signals directly to the liver. The liver responds by resisting insulin’s “stop making glucose” command, cranking out more glucose and VLDL triglycerides. That hepatic insulin resistance then “spills over” system-wide, driving higher fasting sugars and exaggerated post-meal spikes.
Q-2: How does abdominal fat change hormones and chemical messengers that control blood sugar?
A-2: As visceral fat expands, it shifts the adipokine profile: adiponectin (insulin-sensitizing) falls while pro-inflammatory cytokines rise. Leptin climbs but the brain becomes less responsive to it (leptin resistance), dulling appetite and fat-burning signals. Belly fat also boosts local cortisol generation and sympathetic tone, both of which push the body toward insulin resistance.
Q-3: What’s the link between belly fat and “fat in the wrong places,” like the liver and muscles?
A-3: When visceral stores overflow, excess fatty acids deposit ectopically—inside liver cells and skeletal muscle. Lipid intermediates such as diacylglycerols and ceramides interfere with insulin signaling at the cell membrane and mitochondria. The result is a self-reinforcing loop: poorer glucose uptake by muscle, more liver glucose production, and rising triglycerides, even before fasting glucose looks abnormal.
Q-4: How can I recognize abdominal-fat-driven insulin resistance before a diabetes diagnosis?
A-4: Simple clues help: a waist-to-height ratio above ~0.5, a high triglyceride-to-HDL pattern, mild ALT elevation, intense post-meal sleepiness, and dark, velvety skin patches at the neck/underarms (acanthosis). Fasting glucose may still be “normal,” while a 1-hour glucose after a carb-rich meal (or a continuous glucose monitor trace) reveals frequent spikes—an early red flag that the liver and muscle are ignoring insulin.
Q-5: What reliably shrinks visceral fat and reverses the slide toward type 2 diabetes?
A-5: Aim for a 5–10% weight reduction with a modest calorie deficit, but structure matters: prioritize protein (about 1.6–2.2 g/kg/day as appropriate), 25–40 g fiber/day, and minimally processed carbs around activity. Add resistance training 2–3×/week plus 150–300 minutes/week of aerobic work; even 10–15-minute walks after meals lower post-meal glucose by shuttling it into muscle. Protect sleep (7–9 hours), curb late alcohol and sugary drinks, and manage stress (brief breathing or mindfulness breaks). For some, clinician-guided therapy (e.g., targeting weight, liver fat, or insulin sensitivity) is appropriate—especially when strong family history or early glucose abnormalities are present.
Takeaway: Abdominal fat drives insulin resistance through direct liver exposure, inflammatory signaling, and ectopic fat storage. Catch it early with waist-centric measures and lipid patterns, then attack it with protein- and fiber-forward eating, smart training, post-meal movement, and sleep—small, consistent changes that disproportionately deflate visceral fat and improve glucose control.

A Path Forward
Abdominal fat is not just an aesthetic issue; it is a metabolic ticking time bomb. By understanding the link between visceral fat and type 2 diabetes, you can take proactive steps to protect your health.
Start with small, manageable changes—whether it is swapping sugary snacks for fruits, incorporating 20 minutes of exercise into your day, or simply getting enough sleep.
Over time, these habits will not only reduce your abdominal fat but also improve your overall well-being.
Remember, it is never too late to reclaim your health.
Take it one step (or one healthy meal) at a time. Your future self—and your pancreas—will thank you!
References: