It all started when I found myself gaining weight despite sticking to a pretty strict diet and regular exercise routine.
My energy was low, my clothes felt tighter, and my frustration was sky-high.
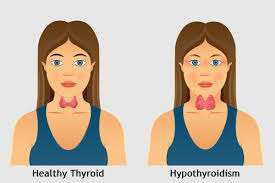
That is when my doctor suggested testing for hypothyroidism, a condition where the thyroid gland does not produce enough hormones, which can slow down metabolism and cause weight gain.
At first, I did not understand how a tiny gland in my neck could lead to such big changes in my body.
But as I dug deeper, I began to see how hypothyroidism can truly hijack your metabolism, making it harder to maintain or lose weight.
This article will explore how hypothyroidism slows down metabolism and leads to weight gain, based on personal experience and supported by science.
Points Covered in this Article:
- Understanding Hypothyroidism and Its Role in Metabolism
- How Hypothyroidism Lowers Basal Metabolic Rate (BMR)
- The Link Between Hypothyroidism and Fatigue
- Hashimoto’s Disease and Its Impact on Metabolism
- Hypothyroidism’s Role in Appetite and Food Cravings
- Why Weight Gain Happens Despite a Healthy Lifestyle
- Hypothyroidism and Its Effect on Muscle Mass
- FAQs on Hypothyroidism and Weight Gain
- Can Treating Hypothyroidism Help Reverse Weight Gain?
- Conclusion: Hypothyroidism, Metabolism, and Weight Gain
Understanding Hypothyroidism and Its Role in Metabolism
When we talk about hypothyroidism, we’re essentially discussing how the thyroid gland fails to produce enough thyroid hormones—mainly triiodothyronine (T3) and thyroxine (T4).
These hormones are crucial for regulating your body’s metabolic processes.
If they are in short supply, your body shifts into a slower gear, and this is where the trouble starts.
In my case, the lack of energy I felt was directly linked to my low thyroid hormone levels.
Without enough of these hormones, your metabolic engine runs sluggishly.
This condition, known as hypothyroid and metabolism dysfunction, results in slower energy usage and makes weight management a real challenge.
How Hypothyroidism Lowers Basal Metabolic Rate (BMR)?
Basal Metabolic Rate (BMR) is the amount of energy your body expends at rest just to stay alive—think of it as the energy needed to keep your heart beating, lungs breathing, and cells functioning.
It accounts for 60–75% of daily calorie expenditure, making it a major player in weight management.
But when hypothyroidism enters the scene, it throws a wrench into this finely tuned system.
Thyroid Hormones: The Master Regulators of Metabolism
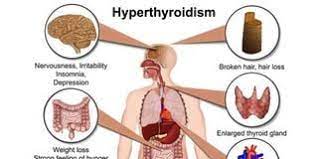
Your thyroid gland produces two main hormones—T3 (triiodothyronine) and T4 (thyroxine). These hormones regulate how your body uses energy. In hypothyroidism, T3 and T4 levels are low, causing every system—especially your metabolism—to slow down.
Multiple studies, including a meta-analysis in The Journal of Clinical Endocrinology & Metabolism, confirm that people with untreated hypothyroidism can experience up to a 20–40% drop in BMR depending on the severity.
That means your body burns significantly fewer calories just to keep itself running—even when you are doing nothing.
Cold Hands, Weight Gain, and Fatigue: Real Signs of Slowed BMR
When your BMR drops, your body conserves energy. You may feel colder, more fatigued, and experience unexplained weight gain.
I remember struggling with cold extremities and exhaustion—even though I was sticking to a clean diet and hiking trails for weight loss. My weight refused to budge until my thyroid was brought under control.
Why the Scale Won’t Budge—Even with Diet and Exercise
A low BMR means your body is working with a reduced calorie budget. For example, someone whose normal BMR is 1,500 calories a day might drop to just 1,200 with hypothyroidism.
That 300-calorie difference adds up quickly—especially when combined with fatigue that makes working out harder.
Even mild hypothyroidism, known as subclinical hypothyroidism, has been linked to modest weight gain and reduced metabolic function in longitudinal studies like those published in Thyroid Research.
The Good News: BMR Can Recover With Treatment
With proper thyroid hormone replacement therapy—usually levothyroxine—BMR can gradually return to normal.
Studies show that restoring thyroid levels often leads to weight stabilization, improved energy, and a gradual increase in resting calorie burn.
If you are battling stubborn weight and suspect a sluggish thyroid, a simple blood test can offer powerful insight.
The Link Between Hypothyroidism and Fatigue
Feeling constantly tired?
You are not alone.
One of the most frustrating symptoms of hypothyroidism is chronic fatigue.
It is a double-edged sword: your metabolism is already slow, and on top of that, hypothyroidism saps your energy, making it difficult to stay active.
I noticed this cycle firsthand. The fatigue that comes with hypothyroidism often made it harder to stick to my usual bodyweight workout routine. This lack of physical activity only worsened my weight gain.
According to studies published in the Thyroid Research Journal, the constant fatigue associated with hypothyroidism makes it difficult for people to engage in enough physical activity to burn calories effectively, further contributing to obesity in hypothyroidism.
Hashimoto’s Disease and Its Impact on Metabolism
For many people, hypothyroidism is caused by Hashimoto’s disease, an autoimmune disorder where the immune system attacks the thyroid gland.
Hashimoto’s and obesity often go hand in hand because, like hypothyroidism, the disease leads to lower thyroid hormone levels and a subsequent slowdown in metabolism.
When I was diagnosed with Hashimoto’s, I began to understand why weight gain was so stubborn for me.
Hashimoto’s and metabolism are closely linked, as the body’s autoimmune attack reduces the thyroid’s ability to function, slowing down the body’s ability to burn calories and store fat efficiently.
Studies have shown that Hashimoto’s patients often experience higher rates of weight gain and difficulty losing weight compared to those with standard hypothyroidism (American Thyroid Association).
Hypothyroidism’s Role in Appetite and Food Cravings
Hypothyroidism, characterized by an underactive thyroid gland, can subtly influence weight gain by affecting appetite and food cravings. Your body’s fat storage is determined by thyroid and hence, this gland is vital for effective weight management.
The thyroid gland produces hormones that regulate metabolism, and when these hormones are deficient, metabolic processes slow down, leading to various physiological changes.
Increased Cravings for Carbohydrates and Sugars:
A sluggish metabolism resulting from hypothyroidism can disrupt the body’s energy balance, often leading to increased cravings for carbohydrates and sugars.
This craving is the body’s attempt to seek quick energy sources to counteract feelings of fatigue associated with a slower metabolic rate.
Personally, I’ve noticed that despite my efforts to maintain a balanced diet, I tend to crave more carbs, especially during periods of low energy.
Impact on Appetite-Regulating Hormones:
Research indicates that hypothyroidism can alter the levels of hormones responsible for appetite regulation, such as leptin and ghrelin. Leptin, produced by fat cells, signals satiety to the brain, while ghrelin, produced in the stomach, stimulates hunger.
In hypothyroid individuals, leptin levels may be elevated, but the brain’s sensitivity to leptin can be reduced, leading to persistent feelings of hunger and increased food intake.
Fatigue and Its Influence on Eating Habits:
Fatigue is a common symptom of hypothyroidism and can significantly impact eating behaviors.
When energy levels are low, there is a natural tendency to seek out high-energy foods, particularly those rich in sugars and simple carbohydrates, as they provide rapid, albeit temporary, energy boosts.
This pattern can contribute to weight gain over time.
Managing Appetite and Cravings:
Effectively managing hypothyroidism involves more than just hormone replacement therapy; lifestyle and dietary modifications play crucial roles. Thyroid hormone deficiency leads to weight gain, that can be avoided if you are careful of your health.
Here are some strategies that have proven helpful:
-
Balanced Diet: Focus on a diet rich in complex carbohydrates, lean proteins, healthy fats, and fiber. Complex carbs, found in whole grains and vegetables, provide sustained energy and help regulate blood sugar levels, reducing sudden cravings.
-
Regular Physical Activity: Engaging in regular exercise such as resistance band squats can boost metabolism and improve energy levels, which may help mitigate fatigue-induced cravings.
-
Mindful Eating: Paying attention to hunger and fullness cues can prevent overeating. Mindful eating practices encourage better food choices and enhance meal satisfaction.
-
Adequate Sleep: Ensuring sufficient and quality sleep is vital, as sleep deprivation can disrupt appetite-regulating hormones, leading to increased hunger and cravings.
It is essential to work closely with healthcare providers to tailor these strategies to individual needs, ensuring a comprehensive approach to managing hypothyroidism and its effects on appetite and weight.
Why Weight Gain Happens Despite a Healthy Lifestyle?
Perhaps one of the most frustrating aspects of hypothyroidism and overweight conditions is how weight gain can occur even if you are doing everything “right.”
Eating a healthy diet and maintaining regular exercise can still lead to disappointing results because hypothyroidism disrupts your body’s normal metabolic functions.
In my own journey, it took me months to realize that despite my efforts, my weight gain was not due to poor choices but because of the underlying issue—hypothyroidism.
Studies in the Journal of Clinical Endocrinology have shown that obesity due to hypothyroidism is often a result of reduced calorie-burning efficiency, which makes losing weight through traditional methods much harder.
Hypothyroidism and Its Effect on Muscle Mass
As per LeanAndFit research, “What many people do not realize is that hypothyroidism also affects muscle mass. Hypothyroidism slows metabolism, but it can also contribute to muscle loss, which further lowers the body’s ability to burn calories”.
Muscle tissue is metabolically active, meaning it burns more calories than fat, even when you’re at rest.
I noticed a decrease in muscle strength when my hypothyroidism was at its worst, and this contributed to my overall weight gain.
Studies have found that reduced thyroid hormone levels can lead to muscle wasting, particularly in severe cases of hypothyroidism (Journal of Clinical Investigation).
This muscle loss not only decreases your BMR but also makes physical activity more challenging, creating a vicious cycle.
FAQs on Hypothyroidism and Weight Gain
Q-1: Is weight gain from hypothyroidism mostly fat—or something else?
A-1: Not all added pounds are fat. Low thyroid hormone reduces protein turnover and raises tissue glycosaminoglycans, pulling water into skin and muscle (myxedema). That fluid retention plus slower gut transit can add 1–5 kg before body fat meaningfully changes. As symptoms persist, reduced thermogenesis and activity nudge true fat mass up—so early treatment often sheds fluid first, then gradually normalizes body composition.
Q-2: Which parts of metabolism does hypothyroidism hit hardest—BMR, NEAT, or the “after-meal burn”?
A-2: All three, but differently. Basal metabolic rate (BMR) drops as mitochondrial output and sodium–potassium pump activity slow. Non-exercise activity thermogenesis (NEAT) falls because fatigue, joint stiffness, and low mood shrink spontaneous movement. Diet-induced thermogenesis (the “after-meal burn”) also dips as protein synthesis and sympathetic tone decline. The triple hit explains why weight gain can creep in even without intentional overeating.
Q-3: Why do I feel less hungry yet still gain?
A-3: Thyroid hormones amplify sympathetic signals that keep you warm and active. When they’re low, you move less, run colder, and may choose energy-dense “comfort” foods, especially in the evening. As per leanandfit.info, “Leptin can run relatively high for your fat mass, but the brain’s responsiveness is blunted—so satiety cues feel unreliable”. Net result: small intake increases plus sizable output decreases—an unfavorable energy gap without obvious appetite spikes.
Q-4: How does hypothyroidism change where I store weight and how my blood lipids look?
A-4: With lower T3 activity, brown and beige fat burn less, so less energy is wasted as heat. The liver clears LDL particles more slowly and makes fewer bile acids, pushing LDL-C (and often total cholesterol) up. Many people notice central weight gain with cooler hands/feet and rising LDL; treating the thyroid problem often improves lipids alongside energy and body temperature.
Q-5: If I start levothyroxine, how quickly should weight and metabolism rebound—and what can I do meanwhile?
A-5: Fluid shifts can improve within weeks, but full metabolic recovery tracks dose titration and steady TSH/T4 levels—often 6–12 weeks. While medication stabilizes, maximize “metabolic levers”: protein-forward meals, consistent sleep, and gentle progression of activity (daily walks using step tracking, then 2–3 light resistance sessions). These raise NEAT and preserve lean mass so BMR can climb back. If labs normalize but weight stalls, review dose timing (empty stomach, away from calcium/iron) and reassess total energy balance.

Can Treating Hypothyroidism Help Reverse Weight Gain?
While hypothyroidism causes obesity, treating the condition can sometimes help in reversing the weight gain.
Once I started treatment with thyroid hormone replacement, I noticed that my energy levels improved, and my ability to lose weight gradually returned. However, it’s important to note that treatment alone does not guarantee significant weight loss.
Many people, including myself, find that losing weight post-treatment is still slower compared to those with normal thyroid function.
Research from the Endocrine Society suggests that while thyroid hormone replacement helps restore normal metabolism, many patients still experience difficulty achieving their pre-diagnosis weight.
This is partly because the body adjusts to the slower metabolism over time, and metabolic recovery can be gradual.
Hypothyroidism, Metabolism, and Weight Gain – The Uncanny Connection
In conclusion, hypothyroidism slows down metabolism, leading to weight gain through several mechanisms.
From reducing the basal metabolic rate to altering hormonal balance, this condition makes it harder to burn calories and easier to store fat. Add in the constant fatigue and muscle loss that often accompany hypothyroidism, and weight gain can feel inevitable.
In my experience, even with the best intentions, managing weight with hypothyroidism can be an uphill battle.
That said, understanding the root cause of the weight gain is empowering.
The key is patience, consistency, and working with your healthcare provider to find the right balance of treatment and lifestyle adjustments to keep your weight and health in check.
References: