A recent study published in the International Journal of Obesity emphasizes the need for targeted screening for Cushing’s syndrome among individuals with metabolically unhealthy obesity (MUO).
This large-scale research, conducted between December 2020 and June 2022, involved over 1,000 patients and found that selective screening could significantly increase the likelihood of accurate diagnosis for this rare endocrine disorder.
Understanding Cushing’s Syndrome and Its Impact on Obesity
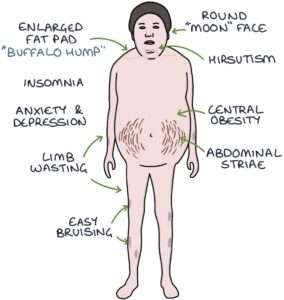
Cushing’s syndrome is characterized by an overproduction of the hormone cortisol, either due to endogenous factors such as tumors in the adrenal or pituitary glands, or exogenous factors like prolonged use of glucocorticoid medications.
This hormonal imbalance can lead to various symptoms, including severe weight gain, especially around the upper body, muscle weakness, and high blood pressure.
While Cushing’s syndrome is relatively rare, it often presents diagnostic challenges due to its overlapping symptoms with other conditions like metabolic syndrome and type 2 diabetes (National Institute of Diabetes and Digestive and Kidney Diseases)
The Study: Key Findings and Implications
The study analyzed data from 1,008 obese patients who underwent screening for Cushing’s syndrome at an endocrinology outpatient clinic.
Participants were categorized into two groups: those with metabolically unhealthy obesity (MUO) and those with metabolically healthy obesity (MHO). The researchers used the 1 mg overnight dexamethasone suppression test (DST) to assess cortisol levels.
A serum cortisol level of ≥1.8 µg/dL indicated a positive test result for Cushing’s syndrome.
The findings were revealing:
- Cortisol Levels in MUO vs. MHO: Patients with MUO had significantly higher cortisol levels compared to those with MHO. Among the entire study group, 12 patients (1.2%) had a cortisol level of ≥1.8 µg/dL, with 11 of these patients belonging to the MUO category.
- Diagnostic Accuracy: The DST showed high specificity (99%) and sensitivity (100%) in diagnosing Cushing’s syndrome among patients with MUO. This highlights the effectiveness of using DST as a screening tool in this population.
- Prevalence and Risk Factors: The overall prevalence of Cushing’s syndrome in the study group was 0.2%. Despite its low prevalence, the condition was more likely to be diagnosed in patients with higher fasting plasma glucose, elevated triglycerides, and low HDL cholesterol levels (International Journal of Obesity, 2024).
Why Targeted Screening is Important
The study’s results suggest that instead of screening all individuals with obesity, a more prudent approach would be to focus on those with MUO. LeanAndFit research staff agrees with this approach.
This strategy not only increases the likelihood of identifying Cushing’s syndrome but also avoids unnecessary testing in those less likely to have the condition.
Given that untreated Cushing’s syndrome can lead to severe complications, including cardiovascular disease and increased mortality, early and accurate diagnosis is crucial (National Institute of Neurological Disorders and Stroke)
Challenges in Diagnosing Cushing’s Syndrome
Diagnosing Cushing’s syndrome can be complex due to its symptom overlap with other conditions.
Traditional diagnostic methods, such as the 24-hour urinary free cortisol test and late-night salivary cortisol test, can sometimes yield ambiguous results.
This complexity is further compounded in patients with obesity, where similar symptoms may be attributed to other metabolic disorders (CDC).
For example, a separate analysis by the Centers for Disease Control and Prevention (CDC) found that metabolic syndrome, characterized by a cluster of conditions such as hypertension, insulin resistance, and abdominal obesity, significantly increases the risk of mortality even in individuals with normal weight.
This highlights the importance of differentiating between metabolic syndrome and Cushing’s syndrome to avoid misdiagnosis and ensure appropriate treatment.
Implications for Clinical Practice
The study underscores the importance of adopting a more targeted and strategic approach when screening for Cushing’s syndrome in obese individuals—particularly those with signs of metabolic dysfunction.
Rather than casting a wide net, clinicians can enhance diagnostic precision by concentrating on patients who meet the criteria for metabolically unhealthy obesity (MUO), a subgroup characterized by insulin resistance, hypertension, dyslipidemia, and visceral adiposity.
This tailored strategy not only conserves medical resources but also facilitates earlier identification of an often-overlooked endocrine disorder. Given the high sensitivity and specificity of the dexamethasone suppression test (DST) in this demographic, the study suggests it could serve as a reliable frontline screening tool in endocrinology practices.
Implementing DST more routinely in MUO cases could lead to earlier diagnoses, better management outcomes, and a reduced burden of comorbidities.
As per recommendations from the National Institutes of Health, aligning screening methods with metabolic risk profiles may redefine how endocrine disorders are detected in obese populations.
The Way Forward
This study provides valuable insights into the selective screening of Cushing’s syndrome in patients with metabolically unhealthy obesity.
While the overall prevalence of the condition remains low, its impact on health outcomes can be profound, making early diagnosis and intervention essential.
Moving forward, further research is needed to refine screening guidelines and explore additional biomarkers that could aid in the accurate detection of Cushing’s syndrome in at-risk populations.
References: