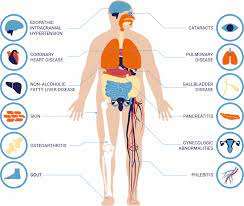
Obesity and Non-Alcoholic Fatty Liver Disease (NAFLD) are closely intertwined health challenges that have become increasingly prevalent in modern society.
NAFLD, characterized by fat accumulation in the liver without significant alcohol consumption, is now recognized as the most common chronic liver disease globally.
In this article, LeanAndFit research team will delve into how and why obesity contributes to NAFLD, examining its mechanisms, risk factors, and progression.
By breaking down the scientific processes and presenting real-life examples, we aim to provide a clear understanding of this critical health connection.
Index
- What Is Non-Alcoholic Fatty Liver Disease?
- The Role of Obesity in NAFLD Development
- How Insulin Resistance Links Obesity and NAFLD
- The Role of Inflammation in Liver Fat Accumulation
- The Impact of Visceral Fat on Liver Health
- Progression from NAFLD to NASH: A Dangerous Path
- Real-Life Example: John’s Struggle with Obesity and NAFLD
- Conclusion: The Crucial Link Between Obesity and Liver Health
What Is Non-Alcoholic Fatty Liver Disease?
NAFLD occurs when excessive fat builds up in liver cells, comprising more than 5–10% of the liver’s weight.
It spans a spectrum of liver conditions, starting with simple steatosis (fat accumulation) and potentially progressing to Non-Alcoholic Steatohepatitis (NASH), fibrosis, and even cirrhosis.
Unlike alcohol-induced liver disease, NAFLD is primarily linked to metabolic dysfunction rather than alcohol consumption.
According to the Journal of Hepatology, NAFLD affects approximately 25% of the global population, with prevalence rates soaring in obese individuals.
This alarming trend underscores the urgent need to understand the connection between obesity and liver health.
The Role of Obesity in NAFLD Development
Obesity is a leading risk factor for Non-Alcoholic Fatty Liver Disease (NAFLD), with research indicating that 70–90% of obese individuals develop fatty liver.
This strong correlation stems from multiple physiological and metabolic mechanisms tied to excessive body fat.
Here is how obesity contributes to NAFLD:
- Excess Caloric Intake: Chronic overconsumption of calories, particularly from high-fat and high-sugar diets, leads to fat accumulation beyond the body’s storage capacity. This excess fat spills over into ectopic sites such as the liver, resulting in hepatic steatosis—a hallmark of NAFLD.
- Dysregulated Fat Metabolism: Obesity disrupts the balance of fat storage, mobilization, and oxidation. The liver becomes overwhelmed with free fatty acids from dietary sources and lipolysis (fat breakdown in adipose tissue), increasing triglyceride storage in hepatocytes.
- Hormonal Dysregulation: Obesity alters the function of key hormones like leptin and adiponectin. Low adiponectin levels in obese individuals impair fat oxidation and anti-inflammatory pathways in the liver, while leptin resistance contributes to chronic inflammation and further fat deposition.
A study in Hepatology highlighted that obesity accelerates NAFLD progression by driving obesity based insulin resistance and inflammation, compounding liver damage over time.
This connection underscores the importance of managing body weight to mitigate NAFLD risk.
How Insulin Resistance Links Obesity and NAFLD
Insulin resistance is a pivotal mechanism connecting obesity to Non-Alcoholic Fatty Liver Disease (NAFLD).
When the body becomes resistant to insulin, the hormone fails to regulate glucose and fat metabolism effectively, setting off a chain reaction that directly impacts liver health.
Here is how:
- Increased Lipogenesis: Insulin resistance triggers de novo lipogenesis, a process where the liver converts excess dietary sugars into fat. This leads to fat accumulation in liver cells, a defining feature of NAFLD.
- Reduced Fat Export: Insulin resistance hampers the liver’s ability to package and export triglycerides as very-low-density lipoproteins (VLDLs). As a result, triglycerides accumulate, exacerbating hepatic steatosis.
- Decreased Fat Oxidation: The liver’s capacity to burn stored fat for energy is reduced in obese individuals with insulin resistance. This imbalance further accelerates fat buildup in the liver.
A study in Diabetes Care found that insulin resistance is the strongest predictor of NAFLD in both adults and children, emphasizing its central role.
This metabolic dysfunction not only links obesity and liver disease but also creates a vicious cycle, as fat accumulation worsens insulin resistance, driving the progression of NAFLD to more severe stages like NASH (Non-Alcoholic Steatohepatitis).
The Role of Inflammation in Liver Fat Accumulation
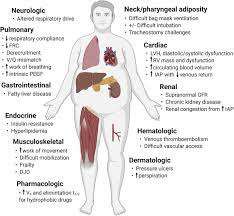
Obesity is closely linked to chronic low-grade inflammation, a key factor in the development and progression of liver diseases such as Non-Alcoholic Fatty Liver Disease (NAFLD).
Adipose tissue in obese individuals acts as an endocrine organ, releasing pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). These inflammatory markers contribute to liver damage in several ways:
- Promote Liver Damage: Chronic inflammation caused by cytokines directly damages hepatocytes (liver cells), facilitating the progression from simple fat accumulation (NAFLD) to more severe conditions like Non-Alcoholic Steatohepatitis (NASH).
- Disrupt Insulin Signaling: Inflammatory cytokines interfere with insulin pathways, exacerbating insulin resistance. This disruption increases glucose levels and accelerates hepatic fat accumulation.
- Initiate Fibrosis: Long-term inflammation activates hepatic stellate cells, triggering the formation of fibrous tissue. This scar tissue can eventually lead to cirrhosis and liver failure.
A study in Hepatology highlighted that inflammatory markers in obese patients were significantly correlated with advanced liver damage, underscoring the critical role of inflammation in liver fat accumulation and its complications.
The Impact of Visceral Fat on Liver Health
Visceral fat, the fat stored around abdominal organs, is particularly harmful to liver health due to its high metabolic activity.
Unlike subcutaneous fat, visceral fat releases inflammatory cytokines and free fatty acids directly into the liver through the portal vein, creating a cascade of negative effects:
- Increased Liver Fat Storage: Free fatty acids released from visceral fat are absorbed by the liver, contributing to hepatic fat accumulation. Over time, this leads to the development of Non-Alcoholic Fatty Liver Disease (NAFLD).
- Higher Risk of NASH: Individuals with elevated visceral fat are significantly more likely to experience inflammation and progress from simple steatosis to Non-Alcoholic Steatohepatitis (NASH), a more severe form of liver disease.
- Endocrine Disruption: Visceral fat produces hormones and cytokines such as adiponectin, leptin, and TNF-α, which impair insulin sensitivity and exacerbate liver inflammation and fibrosis.
A study published in The Lancet found that visceral fat levels are a stronger predictor of liver fat accumulation than subcutaneous fat, underlining the dangers of abdominal obesity.
This unique relationship between visceral fat and liver health highlights the critical need to address central obesity in managing and preventing liver-related complications.
Progression from NAFLD to NASH: A Dangerous Path
Non-Alcoholic Fatty Liver Disease (NAFLD), while often benign in its early stages, has the potential to progress to Non-Alcoholic Steatohepatitis (NASH), a more severe condition characterized by liver inflammation and cell damage.
Alarmingly, approximately 20% of NAFLD cases advance to NASH, significantly increasing the risk of fibrosis, cirrhosis, and liver failure.
Obesity plays a critical role in accelerating this progression through multiple mechanisms:
- Amplifying Oxidative Stress: Obesity increases the production of reactive oxygen species (ROS) due to excess fat in liver cells. These ROS damage the liver’s DNA, proteins, and lipids, further exacerbating cell dysfunction and death.
- Worsening Inflammation: The chronic low-grade inflammation associated with obesity releases pro-inflammatory cytokines like TNF-α and IL-6. These cytokines promote liver inflammation, hastening the transition from simple steatosis to NASH.
- Reducing Repair Mechanisms: Prolonged metabolic stress in obese individuals impairs the liver’s ability to repair itself. Hepatocytes lose their regenerative capacity, while activated stellate cells promote scar tissue formation, leading to fibrosis.
A study in Hepatology highlighted that individuals with obesity are twice as likely to develop NASH compared to non-obese individuals, emphasizing the critical link between body weight and liver health.
Early diagnosis and intervention in NAFLD are vital to prevent this dangerous progression.
John’s Struggle with Obesity and NAFLD
John, a 45-year-old office worker, had struggled with being overweight for most of his adult life.
A sedentary lifestyle combined with a diet heavy in fast food and sugary drinks made weight management a challenge.
Despite these habits, John rarely felt unwell and assumed his health was intact—until routine blood tests showed elevated liver enzymes.
Concerned, his doctor ordered an ultrasound, which confirmed that John had Non-Alcoholic Fatty Liver Disease (NAFLD).
During their consultation, John’s doctor explained how obesity played a critical role in the development of NAFLD.
His visceral fat, the harmful fat stored around abdominal organs, was releasing inflammatory cytokines and driving insulin resistance.
These metabolic disturbances caused fat to accumulate in his liver, leading to fatty liver disease.
Motivated to improve his health, John worked with a nutritionist to adopt a balanced, calorie-conscious diet.
He also began incorporating light daily exercises, such as walking and yoga, into his routine.
Over the course of a year, John lost 15% of his body weight.
Follow-up tests showed dramatic improvements: his liver enzymes normalized, and his ultrasound revealed significant reduction in liver fat.
John’s transformation illustrates how addressing obesity through lifestyle changes can effectively combat NAFLD and improve overall health.
The Crucial Link Between Obesity and Liver Health
The relationship between obesity and NAFLD is both direct and multifaceted, involving mechanisms like insulin resistance, inflammation, and visceral fat deposition.
This strong connection underscores the importance of addressing obesity as a primary strategy to prevent and manage NAFLD.
Understanding this link not only aids in better management of liver health but also highlights the broader implications of metabolic health.
For those at risk, early interventions focusing on weight management, healthy diet, and regular exercise can make a transformative difference.
References: