Gastric bypass surgery, one of the most well-known types of bariatric procedures, is often hailed as a life-changing solution for severe obesity.
For many people struggling with weight loss, it offers the promise of dramatic results and improved health. However, like any medical intervention, it comes with its own set of risks and potential complications.
So, is gastric bypass truly a safe cure, or is it a risky bet that could lead to unforeseen consequences?
In this article, leanandfit.info will dive into the benefits, risks, and long-term outcomes of gastric bypass surgery, backed by scientific research, and explore how this surgery stacks up against other weight loss options.
Contents of this Article:
- What is Gastric Bypass Surgery?
- Different Types of Bariatric Weight Loss Surgery
- How Does Gastric Bypass Work?
- Weight Loss After Gastric Bypass Surgery
- Bariatric Surgery for Teenagers
- Most Successful Bariatric Surgery: Is it Gastric Bypass?
- Weight Loss Surgery After Gastric Sleeve
- Risks of Gastric Bypass Obesity Surgery
- RNY Weight Loss Surgery: The Roux-en-Y Laparoscopic Gastric Bypass
- FAQs on Gastric Bypass Obesity Treatment
- Weight Loss Surgery After Gastric Bypass
- Conclusion: Safe Cure or Risky Bet?
What is Gastric Bypass Surgery?
Gastric bypass surgery is a type of weight-loss procedure designed for individuals with severe obesity.
It is a form of bariatric surgery that alters the digestive system to help patients lose weight and manage obesity-related health conditions.
This procedure is often recommended for those who have struggled to lose weight through traditional methods like diet and exercise and who may face serious health risks due to their weight.
By changing the way the stomach and small intestine process food, gastric bypass helps patients consume fewer calories and feel full more quickly.
It is known to promote significant and long-term weight loss while also improving or even resolving conditions such as type 2 diabetes, high blood pressure, and airway obstruction while sleeping.
Due to its effectiveness, gastric bypass is one of the most commonly performed bariatric surgeries worldwide.
However, it is a major surgical procedure that requires lifestyle adjustments and long-term follow-up care to ensure success.
Different Types of Bariatric Weight Loss Surgery
While gastric bypass is a widely known bariatric surgery, several other procedures are available to assist with weight loss.
Here is a friendly overview of the common types:
1. Gastric Sleeve Surgery (Sleeve Gastrectomy):
- Procedure: Involves removing a large portion of the stomach, leaving a banana-shaped “sleeve.”
- Benefits: Reduces stomach size, leading to decreased food intake and appetite.
- Considerations: It’s a permanent procedure and may require vitamin supplementation due to reduced nutrient absorption.
2. Adjustable Gastric Banding:
- Procedure: Places an inflatable band around the upper part of the stomach to create a small pouch.
- Benefits: Limits food intake and can be adjusted or removed as needed.
- Considerations: Requires regular follow-ups for band adjustments and carries a risk of band slippage or erosion.
3. Biliopancreatic Diversion with Duodenal Switch (BPD/DS):
- Procedure: Combines sleeve gastrectomy with rerouting a significant portion of the small intestine.
- Benefits: Leads to substantial weight loss and can improve obesity-related conditions.
- Considerations: Has a higher risk of nutritional deficiencies and requires strict adherence to dietary guidelines and supplementation.
Tips for Choosing the Right Surgery: The best procedure varies based on individual health profiles, weight loss goals, and medical advice. It is essential to consult with a healthcare provider to determine the most suitable option.
Each surgery carries its own benefits and risks, so thorough research and professional guidance are crucial.
Remember, bariatric surgery is a tool to aid in weight loss and requires a lifelong commitment to lifestyle changes, including diet and exercise, to ensure lasting success.
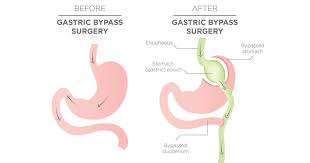
How Does Gastric Bypass Work?
Gastric bypass surgery promotes weight loss through two primary mechanisms, making it one of the most effective bariatric procedures for long-term weight management.
1. Restriction:
- The procedure involves creating a small stomach pouch, significantly limiting the amount of food a person can consume in one sitting.
- Since the pouch holds much less food than a normal stomach, patients feel full faster, helping to control portion sizes and reduce calorie intake.
- This restriction encourages individuals to develop healthier eating habits and avoid overeating, which is crucial for maintaining weight loss over time.
2. Malabsorption:
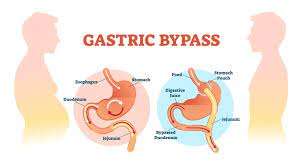
- In addition to reducing stomach size, gastric bypass also involves rerouting a portion of the small intestine, which decreases the absorption of calories and nutrients.
- Since food bypasses part of the digestive tract, fewer calories are absorbed, further promoting weight loss.
- However, this also means the body absorbs fewer essential vitamins and minerals, requiring patients to follow a strict supplementation plan to prevent deficiencies.
Why This Combination is Effective?
- The dual approach of limiting food intake and reducing calorie absorption helps patients lose significant weight quickly while maintaining long-term results.
- Many patients experience 60–80% excess weight loss within the first two years post-surgery.
- While gastric bypass is highly effective, it requires lifelong dietary adjustments, including vitamin supplements, protein-rich meals, and regular medical check-ups to ensure overall health and prevent deficiencies.
With proper adherence to dietary guidelines, gastric bypass can provide lasting weight-loss success and improved overall health.

Weight Loss After Gastric Bypass Surgery
Weight loss after gastric bypass surgery is often rapid and substantial. On average, patients lose 60-80% of their excess weight within the first year after surgery.
However, the amount of weight lost depends on factors like adherence to dietary guidelines, exercise routines, and overall lifestyle changes.
Studies have shown that most patients maintain significant weight loss five to ten years after the procedure, improving their quality of life and reducing obesity-related conditions like diabetes, high blood pressure, and sleep apnea.
Bariatric Surgery for Teenagers
In recent years, there has been growing interest in bariatric surgery for teenagers who are severely obese and at risk of developing life-threatening health conditions.
Gastric bypass and other bariatric surgeries are increasingly being considered as viable options for adolescents, particularly when traditional weight loss methods like diet and exercise have failed.
However, surgery at a young age raises concerns about long-term physical and psychological effects.
LeanAndFit Research suggests that, when carefully selected, teenagers undergoing bariatric surgery can experience substantial health benefits and improved long-term outcomes.
Most Successful Bariatric Surgery: Is it Gastric Bypass?
Gastric bypass is often considered the gold standard in bariatric surgery due to its high success rate and long-lasting results.
Among the different types of bariatric surgeries, it consistently ranks as one of the most successful in terms of sustained weight loss and resolution of obesity-related diseases.
However, the success of the surgery also depends on the patient’s commitment to lifestyle changes post-operation.
While gastric sleeve and other surgeries are effective, gastric bypass remains a popular choice for those seeking significant weight loss with a proven track record of success.
Weight Loss Surgery After Gastric Sleeve
Some patients who undergo gastric sleeve surgery may later opt for a second bariatric procedure, such as gastric bypass, if they experience inadequate weight loss or regain the weight they initially lost.
Weight loss surgery after gastric sleeve is not uncommon, and gastric bypass is often the go-to solution for patients looking to achieve their long-term weight loss goals.
This process, however, comes with added risks due to multiple surgeries and should be carefully evaluated by healthcare providers.
Risks of Gastric Bypass Obesity Surgery
While gastric bypass is effective for many, it is not without risks. Some of the most common complications include:
- Dumping syndrome: A condition where food moves too quickly through the digestive tract, leading to nausea, vomiting, and diarrhea.
- Nutritional deficiencies: Because the surgery affects the body’s ability to absorb nutrients, patients are at risk for deficiencies in vitamins and minerals like iron, calcium, and vitamin B12.
- Ulcers and gallstones: Patients may develop ulcers or gallstones as a result of the surgery.
- Surgical risks: As with any major surgery, there are risks of infection, bleeding, and complications from anesthesia.
Despite these risks, the long-term benefits for patients who commit to lifestyle changes can far outweigh the potential drawbacks.
RNY Weight Loss Surgery: The Roux-en-Y Laparoscopic Gastric Bypass
The Roux-en-Y (RNY) gastric bypass is the most commonly performed type of gastric bypass surgery. It involves creating a small stomach pouch and connecting it to the middle portion of the small intestine (the Roux limb).
This surgery significantly reduces the stomach’s capacity and alters how the body processes food. Performed laparoscopically, it’s a minimally invasive procedure with a faster recovery time compared to traditional open surgery.
RNY weight loss surgery has shown excellent long-term results, with many patients maintaining substantial weight loss and improved health outcomes.
FAQs on Gastric Bypass Obesity Treatment
Q-1: Is gastric bypass a “cure” for obesity or just a tool—and how should I define success?
A-1: Think of it as a durable tool, not a cure. Roux-en-Y bypass rewires gut hormones so hunger drops and fullness signals rise, helping produce large, sustained weight loss. But biology adapts: appetite creeps back, and life habits still matter. A realistic success target is long-term weight reduction with fewer obesity-related complications—not perfection or a forever “off switch.”
Q-2: What risks are unique to bypass versus other bariatric options?
A-2: Bypass adds specific risks: anastomotic leaks/ulcers, internal hernias, strictures, and late reactive hypoglycemia from rapid carbohydrate delivery. Because the duodenum is bypassed, lifelong micronutrient monitoring (iron, B12, calcium, fat-soluble vitamins) is non-negotiable. Sleeve gastrectomy shares some issues but has a different risk mix (e.g., reflux), while adjustable bands have fewer nutrient issues but less durability.
Q-3: How does bypass compare with modern weight-loss medications—safer to try drugs first?
A-3: For many, yes: GLP-1–based and other anti-obesity medications can deliver meaningful loss with fewer irreversible changes. Yet surgery often achieves greater and more durable weight reduction, and can sharply improve diabetes and sleep apnea. A thoughtful sequence is common: optimize lifestyle → try medications → consider surgery if goals or complications remain unmet—especially at higher BMIs or with severe metabolic disease.
Q-4: What does “post-op maintenance” really entail—and why do some patients regain?
A-4: Long-term follow-up is the hidden price of admission. You shall need yearly labs, vitamin repletion, protein-forward eating, resistance training for lean mass and bone, and prompt evaluation of abdominal pain (to rule out internal hernia). Regain usually reflects a blend of biology (hormonal drift), behavior (liquid calories, grazing), and anatomy (pouch/dilation or fistula). Early course-correction keeps results durable.
Q-5: Who might be better off avoiding bypass or delaying it?
A-5: Red flags include uncorrected micronutrient deficiencies, active substance use, untreated eating disorders, severe reflux already controlled by sleeve-unfriendly anatomy, or inability to commit to lifelong follow-up. Women planning pregnancy within a year should delay. If you are thriving on medication plus lifestyle, surgery may be unnecessary now—revisit if weight, comorbidities, or medication tolerance change.
Weight Loss Surgery After Gastric Bypass
In some cases, patients who undergo gastric bypass surgery may require a second procedure if they experience weight regain or complications.
Weight loss surgery after gastric bypass, though rare, is performed to help patients continue their weight loss journey or to correct issues related to the original surgery.
Revisional surgery carries more risks than the initial procedure, so it’s essential to evaluate whether the benefits outweigh the potential complications.
Bariatric Surgery for Morbid Obesity
For patients with morbid obesity—defined as having a body mass index (BMI) of 40 or higher—bariatric surgery offers a potentially life-saving solution.
Gastric bypass and other types of bariatric surgery have been shown to reduce the risk of heart disease, stroke, type 2 diabetes, and certain cancers.
Bariatric surgery for morbid obesity is often recommended when other weight loss methods have failed, and it is considered one of the most effective ways to improve health and longevity for severely obese individuals.
Conclusion: Safe Cure or Risky Bet?
So, is gastric bypass a safe cure or a risky bet for obesity treatment?
The answer depends on the individual. For many patients, gastric bypass has been a life-saving procedure that leads to significant and sustained weight loss, improved health, and a better quality of life.
However, the surgery comes with risks, including potential complications and the need for lifelong lifestyle changes.
Patients considering gastric bypass must weigh the benefits against the risks, seek advice from qualified medical professionals, and commit to the necessary post-surgical care.
Ultimately, while gastric bypass can be a safe and effective cure for obesity, it is not a decision to be taken lightly.
References: