We have all heard the phrase “watch your cholesterol,” but what does it really mean?
For starters, not all cholesterol is bad. LDL cholesterol—often called “bad cholesterol”—gets the most attention because it can build up in the walls of your arteries, leading to health complications like heart disease.
And if you are carrying extra weight, your LDL levels might be higher than they should be. But how exactly does obesity influence LDL cholesterol levels?
In this article, LeanAndFit explore the fascinating relationship between body fat and cholesterol.
We shall break down the science, discuss why losing weight does not always immediately fix the problem, and even examine the difference between hyperlipidemia and obesity.
Let us dive in and demystify the link between obesity and rising LDL cholesterol levels.
Table of Contents:
- What Is LDL Cholesterol?
- The Relationship Between Body Fat and Cholesterol
- How Obesity Increases LDL Cholesterol Levels
- Why Cholesterol Might Go Up After Weight Loss
- The Difference Between Hyperlipidemia and Obesity
- Real-Life Example: Mark’s Cholesterol Wake-Up Call
- Conclusion
What Is LDL Cholesterol?
Before understanding how obesity impacts LDL cholesterol, let’s get acquainted with LDL itself.
LDL stands for low-density lipoprotein, one of the lipoproteins that transport cholesterol in your blood.
Unlike its “good” counterpart, HDL cholesterol, LDL is notorious for depositing cholesterol in the walls of arteries, leading to plaque buildup and an increased risk of heart disease and stroke.
Elevated LDL cholesterol levels, also called hypercholesterolemia, are often influenced by diet, genetics, lifestyle, and—yes—body weight.
The Relationship Between Body Fat and Cholesterol
The connection between body fat and cholesterol is not just about eating fatty foods.
Adipose tissue (body fat) does more than just store energy; it is metabolically active and influences your body’s overall lipid profile.
According to a study in Nature Reviews Endocrinology, obesity is linked to changes in lipid metabolism, including increased LDL cholesterol levels.
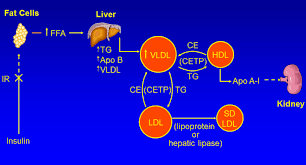
Excess fat tissue promotes the production of very-low-density lipoprotein (VLDL), a precursor to LDL, in the liver.
This chain reaction leads to higher LDL concentrations in the bloodstream.
In simpler terms, the more fat your body carries, the more likely it is to produce LDL cholesterol, which can negatively impact cardiovascular health.
How Obesity Increases LDL Cholesterol Levels?
So, how exactly does carrying extra weight lead to higher LDL cholesterol levels?
Here are the primary mechanisms at play:
- Fat Overload on the Liver: Obesity often leads to fatty liver disease, where excess fat builds up in the liver. This impairs the liver’s ability to regulate cholesterol production and breakdown, resulting in elevated LDL levels.
- Inflammation: Obesity causes chronic low-grade inflammation, which interferes with lipid metabolism. This inflammation can reduce the activity of LDL receptors, making it harder for your body to clear LDL cholesterol from the blood.
- Insulin Resistance: A common companion of obesity, insulin resistance can increase VLDL production in the liver. VLDL eventually converts to LDL, further raising LDL levels in the bloodstream.
A study published in The Lancet Diabetes & Endocrinology found that obese individuals had significantly higher LDL cholesterol levels compared to those with a normal body weight, highlighting the direct impact of excess weight on lipid profiles.
Why Cholesterol Might Go Up After Weight Loss?
You have embraced a healthy lifestyle, cut the junk food, and started shedding pounds—only to discover that your cholesterol levels have climbed.
It might seem disheartening, but this phenomenon is surprisingly common during the early stages of weight loss.
Let’s break it down.
- Fat Mobilization: Weight loss involves burning stored fat, which releases fatty acids and cholesterol into the bloodstream. These fatty acids are transported to the liver, where they are converted into energy or lipoproteins, including LDL cholesterol. This temporary spike is your body’s way of adapting to increased fat breakdown. Over time, as your weight stabilizes, LDL levels typically return to healthier ranges.
- Dietary Changes: Popular weight loss diets like ketogenic or low-carb diet plans are often high in dietary fats. While these diets can improve lipid markers like HDL cholesterol and triglycerides, they can initially raise LDL cholesterol levels. This isn’t always a cause for concern, as other cardiovascular markers often improve simultaneously.
A study in the Journal of the American College of Cardiology found that while LDL levels may rise during weight loss, they usually stabilize or decrease in the long term.
This short-term blip is a normal part of the metabolic adjustment process.
So, if you have wondered, “Why did my cholesterol go up when I lost weight?”—do not panic.
It is likely a temporary phase on your journey to improved health.
Consistency with your healthy habits will eventually lead to better cholesterol levels and overall well-being.
The Difference Between Hyperlipidemia and Obesity
It is common to conflate hyperlipidemia (elevated lipid levels) with obesity, but while the two conditions are often interrelated, they are distinctly different.
- Hyperlipidemia: This condition refers to elevated levels of lipids—cholesterol and triglycerides—in the blood. It can arise from a variety of factors, including genetics, an unhealthy diet, or sedentary habits. However, hyperlipidemia is not exclusive to those who are overweight or obese. Lean individuals can also experience elevated lipid levels due to hereditary conditions or other metabolic factors.
- Obesity: Defined by an excessive amount of body fat, obesity is typically measured using the body mass index (BMI). While obesity often contributes to hyperlipidemia by promoting insulin resistance and increasing LDL cholesterol levels, not all obese individuals will experience abnormal lipid profiles.
A study published in Circulation Research underscores the distinction, noting that while obesity is a significant risk factor for hyperlipidemia, they are separate medical conditions.
This is particularly evident in treatment approaches: weight loss is often recommended for obesity, but managing hyperlipidemia may also require targeted interventions like statins or dietary adjustments, regardless of body weight.
Understanding these differences is vital for tailoring treatment plans and addressing each condition effectively.
By focusing on both lipid levels and body composition, healthcare providers can offer more comprehensive care.
Sophia’s Gestational Diabetes Journey
Sophia, a 34-year-old expectant mother, had struggled with weight management for years.
Her love for processed snacks and long hours at a desk made it hard to maintain a healthy lifestyle.
During her second trimester, a routine glucose tolerance test revealed elevated blood sugar levels, and she was diagnosed with gestational diabetes (GDM).
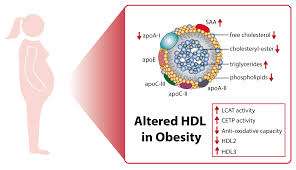
Sophia’s doctor explained that her obesity was a contributing factor, leading to increased insulin resistance and elevated VLDL production, both of which impacted her cholesterol levels.
The diagnosis was a wake-up call; her LDL (“bad” cholesterol) levels were also higher than recommended, posing additional risks during pregnancy.
Determined to ensure a healthy pregnancy, Sophia adopted a balanced diet rich in whole grains, lean proteins, and vegetables.
She also incorporated light exercise, such as daily walks and prenatal yoga.
Initially, Sophia’s blood sugar and cholesterol levels fluctuated due to metabolic adjustments, leaving her frustrated.
However, with consistency and patience, her efforts paid off.
By the third trimester, her LDL cholesterol levels had stabilized, her HDL (“good” cholesterol) levels improved, and her blood sugar remained within target ranges.
Sophia’s story highlights the intertwined relationship between obesity, insulin resistance, and cholesterol during pregnancy, emphasizing the importance of a holistic approach to managing gestational diabetes.
Conclusion
The link between obesity and LDL cholesterol is undeniable.
Obesity disrupts lipid metabolism through mechanisms like fatty liver, inflammation, and insulin resistance, driving up LDL levels and increasing cardiovascular risks.
While weight loss is an essential step toward improving cholesterol, it is important to understand the temporary fluctuations that might occur during the process.
By addressing both obesity and hyperlipidemia, individuals can achieve better overall health and reduce their risk of heart disease.
Awareness, lifestyle changes, and medical guidance are key to navigating this complex relationship and achieving long-term well-being.
References: