Hey there!
If you have ever wondered why obesity often leads to type 2 diabetes or insulin resistance, you are in the right place.
Obesity does not just add pressure on our bodies—it subtly but powerfully rewires how our bodies handle sugar.
This article by leanandfit.info breaks down the complex ways obesity throws glucose metabolism out of sync and explores emerging solutions to help fix it.
Expect a clear, relatable read with science-backed takeaways.
Points Covered in this Article:
- The Basics of Glucose Metabolism
- How Obesity Triggers Metabolic Imbalance
- Insulin Resistance: What Happens and Why
- Fat Tissue, Stress, and Inflammation
- The Deep Dive: Mitochondria and the Randle Cycle
- The Biological Clock and Metabolic Timing
- Hormonal Players: Resistin & Leptin
- Promising Interventions & Hope for Reversal
- FAQs on Obesity & Glucose Metabolism
- Conclusion
The Basics of Glucose Metabolism
Let’s break it down: glucose metabolism is the process your body uses to convert sugar from food into usable energy or store it for later.
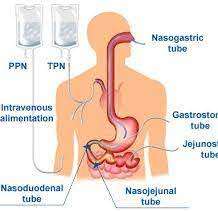
After you eat, carbohydrates are broken down into glucose, which enters your bloodstream. To manage this influx, your pancreas releases insulin—a hormone that acts like a molecular key. Insulin unlocks cells in your muscles, liver, and fat tissue, allowing glucose to enter and be used as fuel or stored for future energy demands.
When everything functions properly, blood sugar levels remain stable and your body runs efficiently. But if this system becomes disrupted—often due to excess fat, inflammation, or hormonal imbalances—cells stop responding well to insulin.
Glucose then lingers in the bloodstream, creating a state of insulin resistance. Over time, this can overwhelm your pancreas and lead to chronically high blood sugar levels, setting the stage for metabolic disorders like prediabetes and type 2 diabetes.
How Obesity Triggers Metabolic Imbalance?
How does obesity throw your metabolism off track?
Let’s use a relatable example. Imagine your fat cells are like storage units. When you gain a little weight, those units just get a bit fuller.
But in obesity—especially with excess belly fat—those storage units burst at the seams. Fat cells (called adipocytes) grow so large that they begin to malfunction.
They do not just store fat—they start releasing stress chemicals and inflammatory signals, like TNF-alpha, that confuse your body’s normal processes. These signals attract immune cells and create chronic, low-grade inflammation.
This environment interferes with insulin, the hormone responsible for allowing sugar into your cells. So even when insulin is present, the cells ignore it—leading to insulin resistance. Over time, glucose builds up in the bloodstream.
This entire chain of dysfunction is what scientists refer to as “obesity glucose metabolism disruption”—a condition where excess fat rewires how your body processes sugar at nearly every level.
Insulin Resistance: What Happens and Why
Here is a quick overview of what insulin resistance stands for and why it happens in the very first place:
Signal Breakdown in Cells:
Under normal circumstances, insulin acts like a key—unlocking cells so glucose can enter and be used for energy.
This process starts when insulin binds to receptors on the cell surface, triggering a series of chemical reactions (called a signaling cascade) that lets glucose in. However, in obesity, things start to break down.
Fat cells release inflammatory molecules like TNF-alpha and IL-6, which interfere with this signaling process.
As a result, the “door” to the cell doesn’t open, even though insulin is knocking.
This cellular refusal is known as insulin resistance—a defining feature of insulin resistance obesity.
The Liver and Sugar Overload:
Meanwhile, the liver gets caught in the crossfire. In people with obesity, the liver tends to accumulate fat—a condition known as fatty liver.
This fatty buildup causes the liver to become insulin resistant too.
But instead of slowing down glucose production, it does the opposite: it keeps making and releasing glucose into the bloodstream, even when there’s already plenty.
This unnecessary glucose release contributes to persistently high blood sugar levels.
Fat Tissue, Stress, and Inflammation
Your lifestyle plays a major role in blood sugar control. Here is a quick explanation of the same:
Meta‑Inflammation:
Obesity leads to meta-inflammation—a chronic, low-grade form of inflammation.
As fat cells expand, they attract immune cells like macrophages, which release inflammatory chemicals such as TNF-alpha.
These signals interfere with insulin’s ability to regulate blood sugar, reducing sensitivity across tissues like muscle and liver.
It is like background noise scrambling a radio signal—insulin is present, but its message is not received.
This widespread inflammation plays a key role in the development of insulin resistance in obesity. It is therefore important to be Lean And Fit in order to regain your lost blood sugar control naturally.
Oxidative Stress:
In obesity, excess fat stresses mitochondria—the cell’s energy producers—leading to oxidative stress.
These overworked mitochondria release reactive oxygen species (ROS), unstable molecules that disrupt insulin signaling and glucose metabolism.
It is like trying to power a city with faulty wiring—systems fail, and energy flow becomes inefficient.
Over time, oxidative stress damages cells and impairs their ability to process glucose properly.
This breakdown contributes significantly to insulin resistance and is a central feature of obesity-related metabolic dysfunction.
The Deep Dive: Mitochondria and the Randle Cycle
Here is how your Mitochondria and Randle cycle jeopardizes your glucose metabolism:
Mitochondrial Breakdown:
In obesity, mitochondria—the tiny power plants inside your cells—begin to falter.
This condition, known as obesity mitochondrial dysfunction, reduces their ability to produce energy efficiently.
As fat accumulates in tissues like muscle and liver, damaged or fragmented mitochondria begin to pile up.
These dysfunctional mitochondria cannot support insulin signaling or glucose processing, contributing to cellular fatigue and poor metabolic performance.
The result is lowered energy output, reduced glucose uptake, and an increased risk of insulin resistance over time.
The Randle Cycle:
When fat stores are excessive, the body shifts its energy preference to burning fat instead of glucose—a mechanism known as the Randle cycle.
In obesity, this shift becomes more pronounced, causing muscle and other tissues to rely heavily on fat metabolism. Glucose then lingers in the bloodstream, raising blood sugar levels.
This Randle cycle obesity pattern interferes with normal insulin function, reinforcing insulin resistance.
Over time, this metabolic shift contributes to poor glucose control and heightened diabetes risk.
The Biological Clock and Metabolic Timing
Every cell in your body operates on a 24-hour rhythm, known as the circadian clock, which helps regulate vital processes like hormone release, energy use, and glucose metabolism.
When your sleep patterns, meal timing, or activity levels don’t align with this internal clock, it can throw your metabolism off balance.
Studies show that disruption of circadian genes—especially BMAL1 in muscle tissue—can impair glucose uptake and insulin sensitivity.
This mismatch between biological timing and lifestyle is at the heart of what researchers call body clock glucose metabolism obesity.
It means that even if you’re eating healthy foods, consuming them at the wrong times (like late at night) can negatively affect how your body handles sugar.
For instance, eating a large meal at midnight may lead to higher blood glucose spikes than eating the same meal at noon. Timing, it turns out, matters just as much as content.
Hormonal Players: Resistin & Leptin
A quick look at how and why your leptin and resistin adversely affects your body’s natural insulin production:
Resistin’s Role:
Resistin is a hormone produced by adipose (fat) tissue, and its levels increase significantly in individuals with obesity.
Elevated resistin appears to interfere with insulin’s ability to regulate blood sugar, contributing to insulin resistance.
This resistin obesity glucose connection is still being explored, but early research indicates that resistin may promote inflammation and disrupt insulin signaling pathways, especially in muscle and liver tissue.
Its role in metabolic imbalance makes it a potential target for future diabetes and obesity treatments.
Leptin’s Disrupted Feedback:
Leptin is a hormone that normally signals the brain to stop eating when fat stores are sufficient.
However, in obesity, this signaling becomes faulty—a phenomenon referred to as leptin resistance that refuses to burn extra body fat.
This leptin reduction glucose dysfunction causes the brain to ignore the “full” signal, leading to continued eating and reduced energy expenditure.
Despite high leptin levels, the feedback loop breaks down, worsening both appetite control and glucose metabolism. This disruption fuels the cycle of weight gain and insulin resistance.
Promising Interventions & Hope for Reversal
Here is how you can hope to regain control over your glucose metabolism:
Weight Loss Can Turn Things Around:
Even moderate weight loss improves insulin sensitivity and lowers blood glucose. Losing just 5–10% of body weight can reverse many of obesity’s effects on metabolism by reducing inflammation and oxidative stress.
Drugs and Medical Therapies:
GLP‑1 agonists (e.g., liraglutide, semaglutide) help reduce appetite, increase insulin action, improve fat tissue health, and even restore leptin signaling. They simultaneously lower glucose and weight, which work hand in hand to rebalance metabolism.
Some newer therapies target mitochondrial health or inflammatory pathways. Early research uses antioxidants to combat ROS in mitochondria or block liver signals that worsen sugar production.
Timing Your Meals:
Time-restricted eating—aligning meals to daylight hours and avoiding late-night eating—can reset your internal clocks, improve insulin sensitivity, and reduce metabolic harm. Simple things like eating breakfast earlier and dinner earlier can make a big difference.
Targeting Specific Tissues:
Scientists are exploring nerve-stimulation techniques to directly improve pancreas or muscle function. Other experimental treatments aim to restore mitochondrial health in muscle—or even tweak circadian proteins—to help reverse glucose disruptions.
FAQs on Obesity & Glucose Metabolism
Q-1: How does excess body fat block insulin’s signal inside cells?
A-1: Enlarged and inflamed fat tissue releases cytokines that switch on stress kinases (like JNK/IKK). These enzymes tag insulin-receptor substrates at the “wrong” sites, so the signal that normally moves GLUT4 to the cell surface is blunted. At the same time, free fatty acids rise and compete with glucose for oxidation (the Randle effect), further lowering muscle glucose uptake. The result is systemic insulin resistance even when insulin levels are high.
Q-2: Why does fat stored in the wrong organs derail glucose control?
A-2: When adipose capacity is exceeded, lipids spill into liver and muscle. In these tissues, lipid by-products such as diacylglycerol activate PKC isoforms that jam insulin receptor signaling, while ceramides hinder Akt—a key step for glucose transport and glycogen synthesis. In the liver, this resistance means unchecked gluconeogenesis and higher fasting glucose; in muscle, it means less meal-time glucose clearance and quicker post-meal spikes.
Q-3: What hormone shifts link obesity to poor glucose handling?
A-3: Adiponectin, which enhances insulin sensitivity and fat burning, typically falls as fat mass rises. Leptin climbs but its brain signal weakens (leptin resistance), eroding appetite control and sympathetic tone that normally supports glucose use. Higher circulating insulin from chronic overnutrition also downregulates its own receptors over time. Add intermittent cortisol surges from chronic stress or sleep loss, and the liver gets a stronger cue to release glucose.
Q-4: How does the gut–liver axis amplify glucose dysregulation in obesity?
A-4: Diet- and obesity-related microbiome shifts can increase intestinal permeability and allow bacterial fragments to reach the liver, stoking low-grade inflammation that worsens hepatic insulin resistance. Altered bile-acid signaling and reduced short-chain fatty acids blunt pathways that usually help muscles and liver handle glucose efficiently. The net effect is a noisier inflammatory background and weaker metabolic “braking,” so blood sugar runs higher on the same foods.
Q-5: Why do daily rhythms and sleep quality matter so much for glucose metabolism in obesity?
A-5: Circadian misalignment (late eating, irregular schedules) desynchronizes clocks in liver, muscle, and pancreas, impairing insulin secretion timing and tissue responsiveness. Sleep restriction and sleep apnea add sympathetic surges and intermittent hypoxia, which raise nighttime glucose production and daytime insulin resistance. Regular meal timing, earlier eating windows, and consolidated 7–9 hour sleep restore clock signals—helping the same calorie intake produce lower glucose and insulin levels.
My Conclusive Analysis
Obesity disrupts glucose metabolism in so many ways: it hampers insulin signals, triggers inflammation, stresses mitochondria, hijacks hormonal balance, and even misaligns your internal clock. The result is a perfect storm that propels insulin resistance, prediabetes, and type 2 diabetes.
But here is the inspiring part: many of these disruptions can be undone. Through weight loss, smart medications, healthier eating patterns, exercise, and better sleep—or even future treatments targeting mitochondria and circadian genes—we have the tools to rebuild healthy sugar control.
Final Takeaways:
- Move: Exercise supports mitochondria, reduces fat, and helps sensitivity to insulin.
- Eat Well & Timely: Focus on balanced meals earlier in the day to sync with your metabolic clock.
- Prioritize Sleep: Good sleep patterns help rebalance leptin, curb inflammation, and support blood sugar control.
- Explore Options: Talk to your provider about GLP‑1 drugs or micro‑step therapies that target metabolic pathways.
- Think Future‑Based: Stay tuned for breakthroughs in mitochondria health and chronotherapy.
Understanding why obesity impairs glucose metabolism empowers you to tackle it effectively—from inflammation and mitochondrial stress to hormone signals and body clocks.
By addressing these root causes, we gain real control—and hope—for reversing insulin resistance and preventing type 2 diabetes.
References: