Breathing is something we take for granted—until it becomes difficult.
The diaphragm, our primary breathing muscle, is responsible for ensuring our lungs fill up with oxygen and deflate like a well-oiled machine.
But what happens when excess fat starts to cramp its style?
Fat accumulation in and around the diaphragm can significantly restrict its movement, making breathing more labored and inefficient.
In this write-up LeanAndFit.info research staff shall dive deep into how fat affects diaphragm movement and why it is important to keep our respiratory system in top shape.
Index:
- Introduction
- The Diaphragm: Your Unsung Hero of Breathing
- How the Diaphragm Moves During Respiration
- The Role of Body Fat in Breathing Mechanics
- How Visceral Fat Affects the Diaphragm
- The Impact of Subcutaneous Fat on Lung Expansion
- Fatty Deposits Around the Rib Cage and Their Role
- Obesity-Related Breathing Conditions
- Strategies to Reduce Fat and Improve Diaphragmatic Function
- FAQs on How Excess Fat Restricts Diaphragm Movement
- Conclusion
The Diaphragm: Your Unsung Hero of Breathing
The diaphragm is a dome-shaped sheet of muscle located just below the lungs. It separates the thoracic cavity (where your lungs and heart reside) from the abdominal cavity.
This muscle plays the lead role in inhalation, contracting to allow the lungs to expand and pulling air into the body.
Without a well-functioning diaphragm, breathing becomes a challenge—think of it like a trampoline with weights sitting on top of it.
Diaphragm breathing restriction due to obesity is a common issue, particularly in individuals carrying excess weight around the midsection.
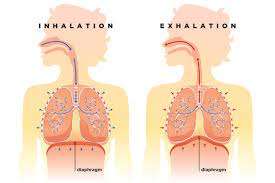
How the Diaphragm Moves During Respiration?
With each inhale, the diaphragm contracts and flattens, allowing the lungs to expand and draw in air. Upon exhalation, it relaxes and returns to its dome shape, pushing air out.
This movement should be smooth and unrestricted.
However, when visceral fat and lung compression occur simultaneously, the diaphragm’s range of motion is reduced, making the simple act of breathing an uphill battle.
Studies have shown that excessive abdominal fat can place mechanical pressure on the diaphragm, limiting its downward movement and reducing lung capacity (Steier et al., 2014).
This restriction forces the body to work harder to maintain adequate oxygen levels, often resulting in shortness of breath, particularly during physical exertion.
Additionally, obesity-related diaphragmatic dysfunction has been linked to decreased chest wall compliance, further impairing normal respiratory mechanics (Pankow et al., 2007).
This explains why individuals with central obesity often experience difficulty taking deep breaths or maintaining steady breathing patterns during activity.
Over time, the continuous struggle to inhale and exhale efficiently can lead to chronic respiratory complications, making weight management a crucial factor in maintaining optimal lung function.
Addressing excess fat through lifestyle modifications can significantly improve diaphragmatic movement, alleviating the breathlessness that often accompanies obesity.
The Role of Body Fat in Breathing Mechanics
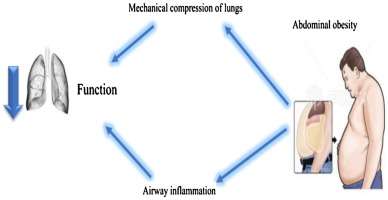
Body fat isn’t just a silent bystander; it can significantly alter breathing mechanics.
The accumulation of fat, particularly in the abdominal and thoracic regions, imposes mechanical restrictions on the chest wall and diaphragm, reducing lung compliance and overall respiratory efficiency.
This leads to diminished lung expansion during inhalation, resulting in lower forced vital capacity (FVC) values.
Additionally, obesity is often associated with chronic low-grade inflammation, which can exacerbate respiratory dysfunction.
These effects are more pronounced in individuals with severe obesity, where the combination of mechanical limitations and metabolic disturbances further compromises lung volumes, increasing the risk of conditions like obesity hypoventilation syndrome and restrictive lung disease.
The distribution of fat plays a crucial role; visceral fat, which surrounds internal organs, is more metabolically active and has been linked to greater respiratory impairment compared to subcutaneous fat, which lies just under the skin.
This fat distribution pattern can lead to decreased lung volumes and increased airway resistance, making each breath less efficient.
Consequently, individuals with central obesity often experience difficulty taking deep breaths or maintaining steady breathing patterns during physical activity.
Over time, this continuous struggle to inhale and exhale efficiently can lead to chronic respiratory complications, underscoring the importance of weight management in maintaining optimal lung function.
How Visceral Fat Affects the Diaphragm?
Visceral fat, the adipose tissue encasing internal organs, poses significant challenges to diaphragmatic movement and overall respiratory mechanics.
Here is how visceral fat accumulation affects the diaphragm:
- Mechanical Restriction: Excess visceral fat in the abdominal cavity exerts upward pressure on the diaphragm, hindering its downward movement during inhalation. This mechanical limitation leads to reduced lung expansion and a persistent sensation of breathlessness, especially during physical activity or when lying down (Pankow et al., 2007).
- Reduced Lung Volumes: The pressure from accumulated visceral fat decreases lung compliance, leading to diminished lung volumes, such as functional residual capacity (FRC) and expiratory reserve volume (ERV). This reduction compromises effective ventilation and oxygenation (Steier et al., 2014).
- Diaphragm Muscle Alterations: Obesity can induce structural and functional changes in the diaphragm muscle, including increased thickness and altered muscle fiber composition. These changes may impair the diaphragm’s contractile efficiency, further compromising respiratory function (Zavorsky et al., 2012).
- Inflammatory Responses: Visceral fat is metabolically active and secretes pro-inflammatory cytokines. This chronic low-grade inflammation can affect respiratory muscles, including the diaphragm, potentially leading to muscle dysfunction and reduced endurance (Pellegrino et al., 2020).
- Orthopnea Development: The upward pressure exerted by visceral fat on the diaphragm is exacerbated when lying down, leading to orthopnea—a condition characterized by shortness of breath in the supine position. This symptom often necessitates sleeping with the head elevated to alleviate discomfort (Benditt, 2017).
- Impaired Diaphragmatic Motion: Visceral fat accumulation can alter the structure of the diaphragm, restricting its motion and contributing to lung function impairment (Lecube et al., 2011).
- Respiratory Muscle Load: The additional mass from visceral fat increases the workload on respiratory muscles, including the diaphragm, leading to quicker muscle fatigue and decreased respiratory efficiency (Parameswaran et al., 2006).
- Compromised Gas Exchange: Reduced diaphragmatic movement can lead to areas of the lungs being under-ventilated, impairing gas exchange and potentially resulting in lower oxygen levels in the blood (Sutherland et al., 2016).
- Altered Breathing Patterns: To compensate for restricted diaphragmatic movement, individuals may adopt rapid, shallow breathing patterns, which are less effective for adequate ventilation and can lead to increased respiratory rate and fatigue (Janssens et al., 2000).
- Increased Risk of Sleep Apnea: Visceral fat accumulation is associated with obstructive sleep apnea, a condition where the airway collapses during sleep, further stressing the diaphragm and compromising sleep quality (Young et al., 2005).
Addressing visceral fat accumulation through lifestyle modifications, such as regular physical activity and a balanced diet, is crucial for improving diaphragmatic function and overall respiratory health (Cleveland Clinic, 2022).
The Impact of Subcutaneous Fat on Lung Expansion
Subcutaneous fat, which sits just under the skin, does not directly press against the diaphragm like visceral fat does.
However, when excessive, it still plays a role in limiting lung expansion. The additional body mass increases the workload on respiratory muscles, making even simple movements like walking or climbing stairs feel disproportionately exhausting.
Studies suggest that excess subcutaneous fat around neck area can lead to reduced chest wall compliance, restricting the natural movement of the ribs and limiting lung inflation.
Furthermore, obesity-related breathing problems often stem from the increased energy demand placed on the body. With more tissue to oxygenate, the respiratory system works harder to maintain normal breathing patterns.
This added strain can contribute to rapid, shallow breathing, reducing the efficiency of oxygen exchange and leading to decreased stamina.
Over time, this extra exertion can cause chronic fatigue, breathlessness, and reduced exercise tolerance, reinforcing a sedentary lifestyle that further exacerbates the issue.
Fatty Deposits Around the Rib Cage and Their Role
Fat can also accumulate around the rib cage, further restricting the lungs’ ability to expand.
The rib cage serves as a critical support structure for respiration, helping to facilitate lung expansion with each breath.
However, when excess fat encases the ribs, it reduces their flexibility, making it harder for the chest to expand fully.
This restriction leads to shallower breaths, limiting the amount of oxygen taken in with each inhale.
Over time, this decreased lung capacity can leave you feeling winded even during light activities, such as talking or walking short distances.
Additionally, the combined effects of impaired diaphragm function and excess abdominal fat can make even sleeping a challenge.
When lying down, the weight of excess fat can press against the chest and diaphragm, increasing the likelihood of sleep disturbances such as obstructive sleep apnea.
This condition leads to interrupted breathing during sleep, further compounding fatigue and respiratory strain.
Obesity-Related Breathing Conditions
When excess fat restricts diaphragmatic movement, it paves the way for a host of breathing-related conditions by impairing lung expansion and increasing the workload on respiratory muscles.
Here are some key conditions linked to restricted diaphragmatic movement:
- Obesity hypoventilation syndrome (OHS): Excess weight places mechanical pressure on the diaphragm, reducing its ability to contract efficiently. This results in shallow breathing, leading to decreased oxygen intake and an accumulation of carbon dioxide in the blood, which can cause headaches, fatigue, and, in severe cases, respiratory failure.
- Sleep apnea: Fat accumulation around the neck and chest increases the risk of airway obstruction during sleep. This leads to episodes of paused or shallow breathing, snoring, poor sleep quality, and excessive daytime fatigue.
- Chronic shortness of breath: With restricted diaphragmatic movement, the lungs struggle to take in adequate air, leaving individuals feeling breathless even during minimal exertion. Over time, this persistent breathlessness can contribute to reduced physical activity and declining cardiovascular health.
How body fat affects oxygen intake is particularly evident in these conditions, as excess tissue increases oxygen demand while simultaneously limiting the diaphragm’s ability to function efficiently.
FAQs on Excess Fat Restricts Diaphragm Movement
Q-1: How does excess abdominal fat affect diaphragmatic movement?
A-1: Excess abdominal fat increases intra-abdominal pressure, which compresses the diaphragm and restricts its downward movement during inhalation. This compression reduces lung expansion, leading to shallow breathing and decreased oxygen intake.
Q-2: In what ways does visceral fat impact diaphragm function?
A-2: Visceral fat, which surrounds internal organs, can infiltrate the diaphragm muscle, leading to structural changes such as increased collagen deposition. These alterations impair the diaphragm’s contractile capacity, resulting in reduced efficiency and potential respiratory dysfunction.
Q-3: How does obesity-induced diaphragm dysfunction affect breathing patterns?
A-3: Diaphragm dysfunction due to obesity can lead to altered breathing patterns, including reduced tidal volume and increased respiratory rate. These compensatory mechanisms aim to maintain adequate ventilation but may not fully offset the mechanical disadvantages imposed by excess fat.
Q-4: What role does increased abdominal pressure play in diaphragmatic restriction?
A-4: Increased abdominal pressure from excess fat compresses the diaphragm, limiting its ability to descend during inhalation. This restriction decreases lung volumes and impairs effective ventilation, contributing to respiratory discomfort and reduced exercise tolerance.
Q-5: How does obesity-related diaphragm dysfunction contribute to sleep-disordered breathing?
A-5: Obesity-related diaphragm dysfunction can lead to reduced diaphragmatic excursion and impaired respiratory muscle strength, increasing the risk of sleep-disordered breathing conditions such as obstructive sleep apnea. This impairment disrupts normal sleep patterns and can lead to daytime fatigue and other health issues.
Q-6: Can weight loss improve diaphragmatic function in obese individuals?
A-6: Yes, weight loss can alleviate the mechanical burden on the diaphragm by reducing abdominal fat. This reduction can enhance diaphragmatic mobility, improve lung expansion, and restore more normal breathing patterns, thereby improving overall respiratory function.
Q-7: Are there specific exercises that can strengthen the diaphragm in obese individuals?
A-7: Breathing exercises, such as diaphragmatic breathing and inspiratory muscle training, can strengthen the diaphragm. Incorporating these exercises into a regular fitness routine may help improve diaphragmatic function and overall respiratory efficiency in obese individuals.
Strategies to Reduce Fat and Improve Diaphragmatic Function
The good news? The effects of excess fat on the diaphragm aren’t irreversible. Here’s how to free up your diaphragm and breathe easy again:
- Lose visceral fat: Since visceral fat is the primary culprit in restricting diaphragmatic movement, focusing on weight loss through a balanced diet and exercise can significantly improve breathing capacity.
- Practice diaphragmatic breathing: Training the diaphragm with deep breathing exercises helps counteract the effects of fat accumulation.
- Increase physical activity: Regular cardio workouts improve lung function and help shed extra pounds, making breathing more efficient.
- Improve posture: Sitting and standing upright allows the diaphragm more room to move, making breathing easier.
- Maintain a healthy sleep position: Sleeping on your side instead of your back can reduce pressure on the diaphragm and make breathing easier at night.
Even small adjustments in lifestyle can lead to noticeable improvements, and strategies to improve diaphragm movement should be a priority for anyone experiencing breathlessness due to excess weight.
Conclusion
Your diaphragm is your breathing powerhouse, but excess fat can put it in a straitjacket, making every breath feel like a struggle.
Visceral fat pushes against it from below, while fat around the rib cage restricts lung expansion, leaving you constantly short of breath.
Even simple activities like walking up stairs or lying down can feel exhausting when your diaphragm is under pressure.
The good news?
Shedding excess fat through exercise (such as sprint interval training), a balanced diet, and better posture can help restore optimal breathing.
So, take a deep breath (if you can) and make those changes—your lungs will thank you for it!
References: