Have you ever wondered how certain medications seem to take the edge off your hunger or make it easier to resist cravings?
These medications, known as appetite suppressants, are specially formulated to help reduce feelings of hunger and support weight loss efforts.
But there is much more going on beneath the surface.
As per leanandfit.info research, “Appetite suppressants do not just affect your willpower—they interact with your body’s intricate hormonal systems, influencing the very signals that tell you when to eat and when you’re full”.
From hunger-regulating hormones like ghrelin to satiety boosters like leptin, these medications create significant shifts in your body’s natural rhythm.
Article Index
- Introduction
A brief overview of appetite suppressants and their influence on hormones. - Understanding Appetite Regulation
- The role of hormones in hunger and satiety
- Key players: Ghrelin and Leptin
- How Appetite Suppressants Work
- Mechanisms of action
- Influence on the central nervous system and fullness signals
- Impact on Ghrelin Levels
- How appetite suppressants affect hunger signals
- The role of lifestyle and exercise
- Influence on Leptin Sensitivity
- Understanding leptin resistance
- Appetite suppressants and improved satiety recognition
- Effects on Other Hormones
- Insulin: Blood sugar and hunger regulation
- Peptide YY (PYY) and GLP-1: Enhancing fullness
- Potential Side Effects and Considerations
- Risks of hormonal imbalance
- Adaptation, dependency, and withdrawal concerns
- Importance of medical supervision
- FAQs on Appetite Suppressants & Hormones
- Conclusion
- Summary of hormonal interactions
- Cautionary advice and importance of professional guidance
Understanding Appetite Regulation
Our body’s hunger and fullness cues are not random—they are tightly regulated by a complex network of hormones working in harmony to maintain energy balance.
Two of the most crucial hormones in this system are ghrelin and leptin, each playing a unique and vital role in appetite regulation.
Ghrelin, often referred to as the “hunger hormone,” is primarily produced in the stomach. Its levels increase before meals, sending a signal to the brain—especially the hypothalamus—that the body needs food. This signal triggers the sensation of hunger. Once we eat, ghrelin levels fall, helping to reduce appetite.
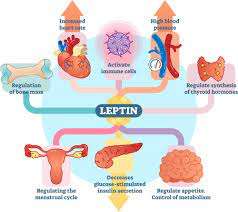
On the other hand, leptin, known as the “satiety hormone,” is produced by fat cells. It communicates with the brain to indicate that energy stores are sufficient, promoting a feeling of fullness and suppressing further eating.
The delicate balance between ghrelin and leptin helps ensure we eat when our bodies need energy and stop when we’ve had enough. If you have leptin resistance then, you cannot lose weight, which is why you continue gaining weight despite exercising regularly.
How Appetite Suppressants Work?
Appetite suppressants are a class of medications commonly used to support weight loss by reducing the urge to eat.
These drugs work by targeting the brain’s appetite control centers, particularly areas in the hypothalamus that regulate hunger and satiety.
By influencing neurotransmitters like serotonin, norepinephrine, and dopamine, appetite suppressants can create a sensation of fullness or diminish the psychological desire to eat, even when physical hunger isn’t present.
Some appetite suppressants work by stimulating the central nervous system, which can lead to a decrease in appetite and an increase in energy expenditure.
Others act more directly on gut hormones or mimic natural signals in the body that promote fullness after eating. So, appetite suppressants curb hunger signals, which is why you are able to maintain an empty stomach for longer duration.
In some cases, these medications may slow down stomach emptying or enhance the release of hormones like GLP-1 and PYY that help suppress hunger.
When used responsibly and under medical supervision, appetite suppressants can be an effective tool in a broader weight management plan.
Impact on Ghrelin Levels:
Some appetite suppressants work by directly influencing ghrelin, the hormone responsible for triggering hunger.
By either reducing the production of ghrelin or blocking its action at the receptor level, these medications can help lower hunger signals sent to the brain.
As a result, individuals feel less compelled to eat, which can aid in calorie reduction and weight loss. Interestingly, ghrelin levels can also be affected by natural lifestyle interventions—particularly intense physical activity.
Studies have shown that exercise, especially at higher intensities, can temporarily suppress ghrelin levels, helping reduce appetite and food intake even after workouts have ended.
Influence on Leptin Sensitivity:
Leptin resistance is a well-documented phenomenon, especially in individuals with obesity.
Under normal conditions, leptin—a hormone produced by fat cells—signals the brain when the body has adequate energy stores, prompting a feeling of fullness and reducing the desire to eat. However, in leptin resistance, the brain becomes less responsive to these signals.
This results in persistent hunger and overeating, even when the body has more than enough stored fat. Some appetite suppressants are designed to help restore leptin sensitivity, allowing the brain to better interpret these satiety cues.
By enhancing leptin’s effectiveness, these medications may help regulate food intake more efficiently. Still, individual responses to these treatments can vary significantly.
Factors such as genetics, metabolic health, and chronic inflammation may influence outcomes.
While the potential is promising, ongoing scientific studies are crucial to fully understand how appetite suppressants interact with leptin signaling pathways and long-term weight regulation.
Effects on Other Hormones
Appetite suppressants influence several additional hormones that play critical roles in hunger regulation and metabolism:
- Insulin
- Regulates blood sugar levels and energy storage.
- Some appetite suppressants may improve insulin sensitivity, making the body more efficient at using glucose.
- Improved insulin function can help stabilize blood sugar levels, reducing sudden hunger spikes and cravings.
- This can also help lower the risk of insulin resistance that causes obesity and type 2 diabetes.
- Peptide YY (PYY)
- A hormone released by the gut after eating.
- Signals the brain to reduce appetite by enhancing the feeling of fullness.
- Some appetite suppressants can increase PYY levels, helping to curb hunger after meals.
- Glucagon-like Peptide-1 (GLP-1)
- Another gut hormone that promotes satiety and slows gastric emptying.
- Enhanced GLP-1 activity can prolong the sensation of fullness, reducing the urge to eat between meals.
- Some modern weight loss medications, like GLP-1 receptor agonists, directly mimic this hormone.
Potential Side Effects and Considerations
While appetite suppressants can offer significant support for weight loss, they are not without potential drawbacks, particularly due to their impact on the body’s hormonal balance.
It is important to consider the following side effects and limitations:
- Hormonal Imbalance
Appetite suppressants alter the levels of key hormones such as ghrelin, leptin, insulin, and serotonin. Over time, this disruption can lead to mood swings, irritability, sleep disturbances, or even metabolic issues like slowed thyroid function. - Short-Term Efficacy
The body may build a tolerance to certain appetite suppressants, especially those that stimulate the central nervous system. This can result in reduced effectiveness over time, making long-term weight maintenance more difficult without additional lifestyle changes. - Dependency and Withdrawal
Some individuals may develop psychological or physical dependence on appetite suppressants. Discontinuing use can lead to withdrawal symptoms, including rebound hunger, fatigue, and weight regain.
For these reasons, medical supervision is essential, along with a holistic plan involving diet, exercise, and behavioral support.
FAQs on Appetite Suppressants & Hormones
Q1: Can appetite suppressants indirectly influence stress hormone (cortisol) levels?
A1: Yes, certain appetite suppressants, particularly those acting on the central nervous system, may indirectly elevate cortisol levels. Since these drugs often stimulate the sympathetic nervous system to reduce hunger, the body’s stress response can be triggered, increasing cortisol secretion. Elevated cortisol can, in turn, affect metabolism and appetite regulation, sometimes counteracting the drug’s intended effects over time.
Q2: Do appetite suppressants affect the balance of sex hormones such as estrogen and testosterone?
A2: Some appetite suppressants may disrupt the delicate balance of sex hormones, especially if used long term. For example, stimulants altering neurotransmitter levels can influence the hypothalamic-pituitary-gonadal axis, potentially lowering testosterone in men or affecting estrogen cycles in women. This hormonal shift could impact energy levels, mood, and reproductive health.
Q3: How might appetite suppressants alter insulin sensitivity beyond appetite control?
A3: Beyond reducing hunger, appetite suppressants can modulate insulin sensitivity by affecting hormone pathways tied to glucose metabolism. Certain suppressants influence hormones like glucagon-like peptide-1 (GLP-1) or leptin, which play roles in insulin regulation. Improved insulin sensitivity might result in better blood sugar control, while altered sensitivity could complicate metabolic health if not monitored carefully.
Q4: Are there appetite suppressants that affect thyroid hormone activity and thus metabolic rate?
A4: Some appetite suppressants may indirectly impact thyroid hormone function by altering pituitary signaling or energy expenditure mechanisms. While they do not typically contain thyroid hormones, these drugs can influence levels of thyroid-stimulating hormone (TSH), potentially modifying metabolism speed. This effect can contribute to weight loss but might pose risks if thyroid function becomes unbalanced.
Q5: Can appetite suppressants interfere with leptin signaling and the body’s natural satiety cues?
A5: Indeed, appetite suppressants often target pathways linked to leptin, a hormone critical for signaling satiety. As per leanandfit.info, “Chronic use can desensitize leptin receptors or disrupt its feedback loop in the hypothalamus, potentially diminishing natural hunger regulation. This interference might lead to rebound hunger or altered eating behaviors once the suppressant is discontinued”.
Conclusion
Appetite suppressants offer a powerful tool in the fight against excess weight by working directly with the body’s complex hormonal systems.
By modifying the levels and activity of key hormones such as ghrelin, leptin, insulin, PYY, and GLP-1, these medications can effectively reduce hunger, enhance feelings of fullness, and help regulate blood sugar—creating an environment more conducive to weight loss.
However, their use is not without risks. The body may adapt over time, diminishing their impact, and hormonal disruptions can lead to unwanted side effects.
Therefore, they should never be seen as a quick fix or standalone solution.
Instead, appetite suppressants should be used thoughtfully and under medical supervision, integrated into a broader, sustainable weight management plan that includes healthy eating, physical activity (such as outdoor trails), and behavioral support (such as cognitive restructuring).
When used wisely, they can help individuals regain control over their appetite and reclaim their long-term health and well-being.
References: