Obesity, a widespread health concern affecting millions worldwide, impacts nearly every system in the body—including the brain.
Recent studies have uncovered a strong link between the chronic inflammation caused by obesity and a heightened risk of dementia, a debilitating neurodegenerative disorder.
This article by leanandfit.info delves into the intricate connection between obesity-related inflammation and dementia, focusing on key mechanisms such as the role of cytokines, insulin resistance, and vascular dysfunction.
To bring these concepts to life, we’ll include real-world examples and evidence-backed insights to provide a clearer understanding of this pressing issue.
Index
- Introduction to Obesity-Related Inflammation and Dementia
- The Role of Chronic Inflammation in the Brain
2.1 Cytokines and Neuroinflammation
2.2 Blood-Brain Barrier (BBB) Dysfunction - Insulin Resistance and Cognitive Decline
- Vascular Dysfunction and Dementia Risk
- Real-Life Examples: Obesity, Inflammation, and Memory Loss
- Scientific Studies Linking Obesity-Related Inflammation to Dementia
- FAQs on Obesity, Inflammation & Dementia
- Conclusion: Understanding the Mechanisms Behind the Connection
Introduction to Obesity-Related Inflammation and Dementia
Obesity sets off a persistent inflammatory response marked by elevated levels of pro-inflammatory cytokines, including interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α).
While these molecules are crucial for fighting infections and facilitating tissue repair, their prolonged activation in obesity creates a harmful environment.
Chronic inflammation disrupts the blood-brain barrier, allowing these cytokines to infiltrate the brain and interfere with normal function.
This sustained inflammatory state accelerates neurodegeneration by damaging neurons and supporting cells, leading to the buildup of toxic proteins such as beta-amyloid and tau—hallmarks of Alzheimer’s disease.
Additionally, inflammation impairs synaptic plasticity, which is vital for learning and memory, further driving cognitive decline.
A study published in Nature Reviews Neuroscience (Miller & Spencer, 2014) found that individuals with obesity had significantly higher levels of neuroinflammation, correlating with an increased risk of dementia.
This highlights the critical role of inflammation in linking obesity to cognitive impairment.
The Role of Chronic Inflammation in the Brain
A quick look at this aspect:
Cytokines and Neuroinflammation
Cytokines released due to obesity-induced inflammation can cross the blood-brain barrier (BBB) and activate microglia, the brain’s immune cells.
Prolonged activation of microglia leads to the destruction of healthy neurons, accelerating cognitive decline.
A study in Nature Neuroscience (Perry et al., 2010) demonstrated that excessive cytokine activity promotes synaptic damage and memory deficits.
Blood-Brain Barrier Dysfunction
The BBB protects the brain from harmful substances in the bloodstream.
Chronic inflammation weakens the BBB, allowing toxins and inflammatory molecules to enter the brain.
Research in the Journal of Neuroinflammation (Banks et al., 2012) found that individuals with obesity have higher levels of BBB permeability, which exacerbates neuroinflammatory processes.
Insulin Resistance and Cognitive Decline
Obesity frequently results in insulin resistance, a condition where cells fail to respond effectively to insulin, a hormone crucial for regulating glucose.
While primarily associated with type 2 diabetes, insulin resistance also significantly impacts brain health.
Insulin in the brain facilitates memory formation, synaptic plasticity, and energy metabolism.
However, when the brain becomes insulin-resistant, its functionality is severely compromised.
Key consequences include:
- Reduced Glucose Metabolism: Insulin resistance disrupts the brain’s ability to metabolize glucose, its primary energy source, leading to cognitive impairments and brain fog.
- Amyloid Plaque Formation: Insulin resistance elevates levels of beta-amyloid, a toxic protein that clumps into plaques, which are hallmark features of Alzheimer’s disease. Insulin dysfunction also impairs amyloid clearance, accelerating neurodegeneration.
A study published in The Journal of Clinical Investigation (Arnold et al., 2014) highlighted a striking link between obesity-induced insulin resistance and Alzheimer’s disease.
The research found that obese individuals with insulin resistance were significantly more likely to develop Alzheimer’s compared to lean individuals.
These findings emphasize the profound role of metabolic health in protecting cognitive function and preventing dementia.
Addressing insulin resistance may be critical for mitigating the cognitive risks associated with obesity.
Vascular Dysfunction and Dementia Risk
Obesity significantly raises the risk of vascular issues such as hypertension, atherosclerosis, and reduced blood flow to the brain, all of which impact cognitive health.
These vascular complications disrupt the brain’s oxygen and nutrient supply, leading to long-term neurological consequences.
Key effects include:
- Ischemic Damage: Insufficient oxygen delivery damages neurons, contributing to vascular dementia, characterized by memory loss and impaired judgment.
- Small Vessel Disease: Obesity-induced vascular dysfunction often results in white matter lesions in the brain. These lesions disrupt communication between different brain regions, causing memory decline and difficulties in executive functioning.
A longitudinal study published in Stroke (Gorelick et al., 2011) identified mid-life obesity as a significant predictor of vascular dementia and Alzheimer’s disease in later years.
The study emphasized the importance of maintaining healthy vascular function to protect brain health.
Addressing obesity’s impact on vascular systems is crucial for reducing dementia risks and preserving cognitive function across the lifespan.
Maria’s Cognitive Struggles: A Turnaround Story
Maria, a 52-year-old teacher, began noticing frequent memory lapses and moments of confusion that interfered with her daily life.
With a BMI of 35, she was classified as obese and presented with elevated inflammatory markers such as IL-6 and TNF-α, along with insulin resistance.
These conditions were putting her at risk for cognitive decline.
After her physician emphasized the link between obesity, inflammation, and brain health, Maria decided to take action.
She adopted an anti-inflammatory diet rich in whole grains, fruits, vegetables, and omega-3 fatty acids.
Combined with regular exercise, these changes led to a 15-pound weight loss over three months.
Alongside the physical benefits, Maria reported significant improvements in her cognitive clarity and overall mental energy.
Tom’s Journey with Early Dementia
Tom, a 60-year-old retired engineer, received a diagnosis of early-stage Alzheimer’s after struggling with frequent forgetfulness and difficulty solving problems.
His medical history revealed a decades-long battle with obesity and hypertension, both significant risk factors for vascular and Alzheimer’s dementia.
Imaging studies showed white matter lesions and reduced brain volume, hallmark indicators of vascular damage and neurodegeneration.
Tom’s neurologist recommended lifestyle changes, including dietary modifications, moderate exercise, and improved blood pressure management.
Over the course of a year, Tom lost 20 pounds and successfully lowered his blood pressure.
While these changes did not reverse his diagnosis, they helped slow the progression of his cognitive decline, providing him with better quality of life and functional independence.
Scientific Studies Linking Obesity-Related Inflammation to Dementia
- Study 1: Nature Neuroscience (Perry et al., 2010)
This study revealed that obesity-induced cytokine elevation directly contributes to synaptic damage and cognitive decline in mice. - Study 2: Journal of Neuroinflammation (Banks et al., 2012)
Demonstrated a correlation between obesity and increased BBB permeability, exacerbating neuroinflammation in humans. - Study 3: The Journal of Clinical Investigation (Arnold et al., 2014)
Identified insulin resistance as a significant factor in beta-amyloid plaque formation, a hallmark of Alzheimer’s. - Study 4: Stroke (Gorelick et al., 2011)
Highlighted the link between mid-life obesity and vascular dementia risk in older adults.
FAQs on Obesity, Inflammation & Dementia
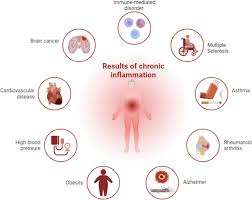
Obesity-related inflammation plays a significant role in the development of dementia through a combination of neuroinflammatory processes, insulin resistance, and vascular dysfunction.
Elevated cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) disrupt brain function by promoting chronic inflammation and oxidative stress, accelerating neuronal damage.
Insulin resistance, often accompanying obesity, impairs glucose metabolism in the brain, contributing to amyloid plaque formation—a hallmark of Alzheimer’s disease.
Additionally, vascular issues such as hypertension and atherosclerosis, frequently linked to obesity, lead to ischemic damage and small vessel disease, further compromising cognitive function.
A study in The Lancet Neurology (Livingston et al., 2020) highlighted that managing obesity can reduce dementia risk by addressing these interrelated mechanisms.
Awareness of this relationship emphasizes the importance of early intervention.
Tackling obesity through lifestyle changes, public health initiatives, and targeted therapies could significantly decrease the prevalence of dementia and improve quality of life for those at risk.
References: