Inflammation is a biological process often linked to obesity and is increasingly recognized for its role in mental health disorders such as depression.
This article delves into the intricate relationship between chronic inflammation caused by obesity and the heightened risk of depression.
We will explore how inflammation affects brain function, the role of inflammatory markers, and the behavioral changes that amplify this connection.
Real-life examples and scientific evidence will provide a comprehensive understanding of this pressing issue.
Article Index
- Understanding the Obesity-Inflammation-Depression Triad
- The Role of Pro-Inflammatory Cytokines in Brain Health
- Neurochemical Disruptions Caused by Obesity-Related Inflammation
- Impact of Chronic Inflammation on the Hypothalamic-Pituitary-Adrenal Axis
- Behavioral and Emotional Pathways Linking Obesity to Depression
- Real-Life Examples: How Inflammation Impacts Mental Well-Being
- FAQs on Obesity and Inflammation
- Scientific Studies on Inflammation, Obesity, and Depression
Understanding the Obesity-Inflammation-Depression Triad
Obesity extends beyond being a physical condition; it triggers a state of low-grade chronic inflammation characterized by elevated levels of pro-inflammatory cytokines, including interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α).
These cytokines travel through the bloodstream and cross the blood-brain barrier, where they disrupt neural processes by altering neurotransmitter pathways and brain function.
How Inflammation Fuels Depression?
The inflammatory cytokines interfere with the regulation of serotonin, dopamine, and other key neurotransmitters, which are essential for mood stabilization.
This disruption not only reduces serotonin synthesis but also contributes to neuroinflammation, a key factor in depressive symptomatology.
Scientific Evidence:
A study published in Brain, Behavior, and Immunity (Miller & Raison, 2016) highlighted the role of inflammation as a critical mediator linking obesity and depression.
The research confirmed that heightened cytokine activity correlates strongly with depressive symptoms, reinforcing the importance of addressing inflammation to manage mental health risks in individuals with obesity.
This evidence highlights the need for a comprehensive approach that addresses both physical and mental health challenges associated with obesity-induced inflammation.
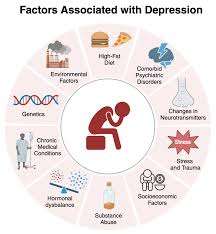
The Role of Pro-Inflammatory Cytokines in Brain Health
Inflammatory cytokines produced by adipose tissue in obesity not only increase systemic inflammation but also impair brain health.
Cytokines like IL-6 and TNF-α disrupt the blood-brain barrier, allowing inflammatory molecules to influence the brain’s microenvironment.
This leads to decreased neurogenesis in the hippocampus, a region critical for regulating mood.
Scientific Evidence
A study in Molecular Psychiatry (Kiecolt-Glaser et al., 2015) demonstrated that individuals with higher levels of inflammatory markers are at a significantly greater risk of developing depression.
The study found that persistent inflammation reduced brain-derived neurotrophic factor (BDNF), which is essential for neuronal survival and plasticity.
Neurochemical Disruptions Caused by Obesity-Related Inflammation
Inflammation profoundly disrupts the balance and synthesis of key neurotransmitters, including serotonin, dopamine, and glutamate.
This imbalance is closely associated with depressive symptoms such as low mood, diminished motivation, and cognitive difficulties.
How It Happens?
Inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), stimulate the enzyme indoleamine 2,3-dioxygenase (IDO).
IDO diverts tryptophan—a critical precursor for serotonin—into the kynurenine pathway, significantly lowering serotonin levels.
Simultaneously, this diversion increases neurotoxic metabolites like quinolinic acid, which exacerbate neuronal damage and depressive symptoms.
Supporting Research
A pivotal study published in Biological Psychiatry (Raison et al., 2010) demonstrated how cytokine-driven alterations in serotonin metabolism contribute to depressive behaviors, particularly in individuals with obesity-induced inflammation.
These findings underscore the biochemical link between systemic inflammation and mood disorders.
Real-World Impact
This mechanism highlights why individuals with chronic inflammation, especially those with obesity, are at greater risk for depression.
Addressing inflammation could mitigate neurotransmitter dysregulation and improve mental health outcomes.
Impact of Chronic Inflammation on the Hypothalamic-Pituitary-Adrenal Axis
The hypothalamic-pituitary-adrenal (HPA) axis is central to the body’s stress regulation.
This system coordinates the release of cortisol, the primary stress hormone, which helps the body respond to acute stress.
However, chronic inflammation, often linked to obesity, disrupts the HPA axis by maintaining prolonged cortisol secretion.
Persistently elevated cortisol levels contribute to depressive symptoms such as fatigue, anxiety, irritability, and difficulty focusing.
Scientific Insight:
A study published in Psychoneuroendocrinology (Rosmond, 2005) demonstrated that individuals with obesity-related inflammation exhibit heightened HPA axis activity.
This overactivation not only exacerbates physical stress but also intensifies psychological stress, creating a self-perpetuating cycle of inflammation and depressive symptoms.
Real-World Relevance
For individuals with obesity, addressing chronic inflammation and restoring HPA axis balance could be crucial in managing both physical health and mental well-being.
The interplay between cortisol and mood highlights the importance of integrative approaches to treatment.
Behavioral and Emotional Pathways Linking Obesity to Depression
Beyond biochemical pathways, behavioral and emotional factors significantly contribute to the connection between obesity and depression.
Social stigma associated with obesity often leads to feelings of isolation, body image issues, and low self-esteem.
These psychological challenges can act as powerful triggers for depressive symptoms.
Additionally, chronic inflammation exacerbates these struggles by heightening emotional sensitivity and reducing an individual’s ability to cope with stress effectively.
Real-Life Example: Emily’s Battle with Stigma and Inflammation:
Emily, a 35-year-old marketing professional, experienced ongoing weight-related discrimination at work.
Subtle remarks and exclusion from team activities caused her to feel isolated and devalued.
This constant stress elevated her inflammatory markers, such as interleukin-6 (IL-6), which further intensified her feelings of hopelessness and sadness.
Her journey toward recovery began with behavioral therapy, which helped her develop coping mechanisms and rebuild her confidence.
Combined with an anti-inflammatory diet and regular physical activity, Emily experienced significant improvements in both her mood and physical health.
Over time, she regained her self-esteem and found a supportive work environment, illustrating how addressing both psychological and physiological factors can break the cycle of obesity-related depression.
Sarah’s Journey with Obesity-Related Depression:
Sarah, a 40-year-old mother, faced daily struggles with obesity and persistent feelings of exhaustion.
Alongside physical discomfort, she began to experience sadness, low energy, and difficulty finding joy in her usual activities.
Concerned about her mental and physical health, Sarah consulted her physician, who ordered blood tests.
The results revealed elevated levels of interleukin-6 (IL-6) and C-reactive protein (CRP), biomarkers associated with systemic inflammation. These findings shed light on the connection between her obesity, inflammation, and depressive symptoms.
With a clear diagnosis, Sarah’s treatment focused on reducing inflammation through dietary changes.
She adopted an anti-inflammatory diet rich in whole foods like leafy greens, nuts, fatty fish, and berries.
She also incorporated daily walks and yoga into her routine. Over time, Sarah noticed a significant improvement in both her mood and energy levels.
John’s Battle with Chronic Stress and Weight Gain:
John, a 50-year-old high school teacher, gained significant weight during a particularly stressful semester.
The demands of his job caused him to adopt poor eating habits, and he became increasingly sedentary.
Soon, John began experiencing mood swings, irritability, and difficulty concentrating. Blood tests revealed elevated inflammatory markers, exacerbating his symptoms.
A combination of cognitive-behavioral therapy (CBT) and anti-inflammatory medications proved transformative.
By addressing his stress and inflammation simultaneously, John regained emotional stability and began adopting healthier lifestyle habits.
Within months, he noticed improvements in his mental clarity and overall well-being.
Scientific Studies on Inflammation, Obesity, and Depression
Study 1: Miller & Raison, 2016 (Brain, Behavior, and Immunity)
This landmark study revealed that chronic low-grade inflammation is a common denominator in obesity and depression, emphasizing the need for integrated treatment approaches.
Study 2: Kiecolt-Glaser et al., 2015 (Molecular Psychiatry)
Highlighted how elevated inflammatory markers in obesity negatively impact hippocampal function, a critical area for mood regulation.
Study 3: Raison et al., 2010 (Biological Psychiatry)
Explored how cytokine-induced changes in serotonin metabolism exacerbate depressive behaviors, shedding light on the biochemical pathways linking inflammation and depression.
Study 4: Rosmond, 2005 (Psychoneuroendocrinology)
Examined the role of cortisol dysregulation in individuals with obesity-related inflammation, providing evidence for its contribution to depression.
Study 5: Puhl & Heuer, 2009 (Obesity Reviews)
Demonstrated the psychological toll of weight stigma, highlighting its role in worsening inflammation and depressive symptoms.
FAQs on Obesity and Inflammation
Q-1: What biological chain links obesity-driven inflammation to a higher risk of depression?
A-1: Visceral fat releases inflammatory messengers that keep the immune system in a low-grade “on” state. Over time, this can weaken the blood–brain barrier, letting more peripheral signals reach the brain. Brain immune cells (microglia, astrocytes) become primed, synaptic connections are stressed, and networks involved in mood regulation work less efficiently. The result is a plausible pathway from central adiposity → chronic inflammation → altered brain signaling → greater likelihood of depressive symptoms.
Q-2: Does inflammation explain specific types of depressive symptoms in people with obesity?
A-2: Often, yes. Inflammation tends to map onto energy-related symptoms: heavier sleep, increased appetite, fatigue, and psychomotor slowing. These features align with immune-metabolic crosstalk that nudges behavior toward conserving energy and seeking calorie-dense foods. In contrast, purely anxiety-like or insomnia-dominant presentations may be less tightly tied to inflammatory tone, which helps clinicians tailor strategies toward metabolic calming when “atypical” symptoms dominate.
Q-3: How do insulin resistance and gut signals fit into the inflammation–depression picture?
A-3: Insulin resistance reduces the brain’s ability to use glucose efficiently and can disrupt reward and motivation circuits. Meanwhile, obesity-linked shifts in gut microbes and intestinal barrier function allow tiny microbial fragments to reach circulation, amplifying immune “noise.” Together, these factors raise inflammatory tone and alter neurotransmission, reinforcing low mood, low drive, and comfort-eating loops that make both weight and mood harder to manage.
Q-4: What everyday patterns quietly raise inflammatory load and, by extension, depression risk?
A-4: Long stretches of sitting, ultra-processed meals rich in refined carbs and fats, short or irregular sleep, and high perceived stress nudge inflammatory markers upward. Even small daily choices—late-night snacking, skipping daylight exposure, inconsistent meal timing—can compound. Over weeks, the immune system’s “idle” creeps up, which can worsen pain sensitivity, sap motivation, and flatten mood—subtle changes that are easy to miss until they add up.
Q-5: Which practical steps can lower inflammation and support mood without waiting months?
A-5: Use a two-track plan. Biologically, shrink visceral fat and calm immune activity with: 10–15 minute walks after meals, two brief resistance sessions weekly, fiber- and protein-forward meals, and consistent 7–8 hour sleep windows. Psychologically, set process goals (steps, meal structure), add brief breathing or mindfulness breaks to downshift stress, and schedule social contact like a weekly walk with a friend. Track a simple trio—waist, sleep duration, and weekly mood score—to see the loop reverse: steadier energy, fewer cravings, and progressively better mood as inflammation cools.
The Inflammation-Depression Link
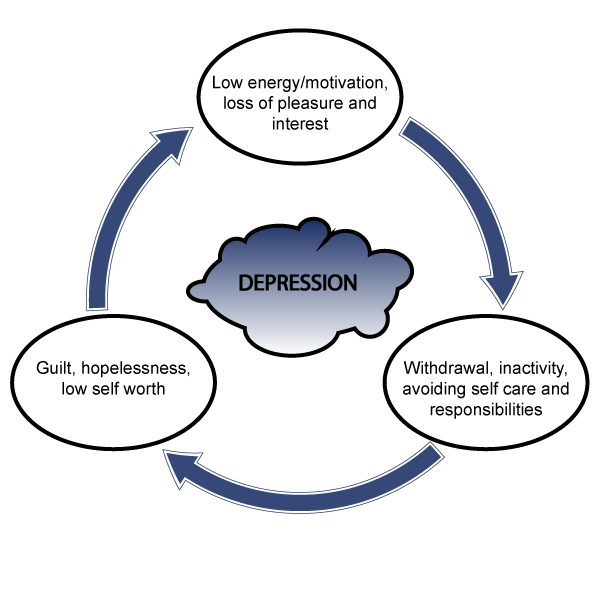
The connection between obesity, inflammation, and depression underscores the importance of addressing both physical and mental health in tandem.
Chronic inflammation disrupts brain function, alters neurotransmitter pathways, and exacerbates emotional challenges, creating a vicious cycle that fuels both obesity and depression.
Continued research and comprehensive treatment strategies are essential for breaking this cycle, offering hope for individuals affected by these interlinked conditions.
By recognizing the role of inflammation in bridging obesity and depression, healthcare providers can adopt more holistic approaches, ensuring improved outcomes for those navigating the challenges of these interconnected health issues.
References: