Imagine this: You are at a buffet, your plate stacked high with everything from pasta to dessert, and your inner voice tells you, “Just one more bite.”
Sound familiar?
For those struggling with obesity, that “one more bite” can turn into a battle of willpower versus hunger.
But what if there were a way to feel satisfied with less food?
Enter the adjustable gastric band, a small but mighty device that has been making big waves in the weight loss world.
In this article, I would break down exactly how this nifty contraption works, explore the science behind it, and sprinkle in some real-life success stories along the way.
Article Contents:
- What Is an Adjustable Gastric Band?
- The Mechanics: How It Works
- Why It’s Adjustable: Customizing the Weight Loss Journey
- Appetite Suppression: The Science Behind Feeling Full
- Real-Life Example: How Sarah Found Freedom from Food Obsession
- Comparing Options: Gastric Band vs. Gastric Sleeve
- The Psychological Aspect: How Eating Habits Are Transformed
- FAQs on Adjustable Gastric Bands to Lose Weight
- Risks and Considerations: It’s Not All Sunshine and Rainbows
- Conclusion: Understanding the Role of Adjustable Gastric Bands
What Is an Adjustable Gastric Band?
First things first, let’s clear up what an adjustable gastric band is.
Picture a rubber band, but for your stomach.
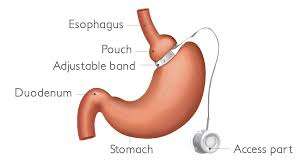
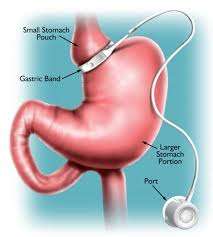
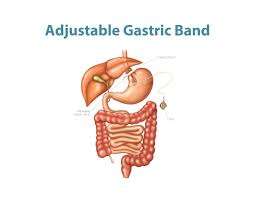
This small, inflatable ring is surgically placed around the upper part of your stomach, creating a smaller pouch above the band.
The result?
You get full faster and eat less, which leads to weight loss.
Unlike more drastic procedures like gastric bypass, this one doesn’t involve slicing and dicing your digestive tract.
It is less invasive, but don’t mistake that for easy.
The Mechanics: How It Works?
So, how does this contraption actually work?
The band is designed to create a bottleneck effect.
The smaller upper stomach pouch fills up quickly, signaling your brain that you’re full.
The food then slowly passes through the narrow opening into the lower part of your stomach.
It is a bit like waiting in line at a crowded theme park ride—slow, steady, and a little frustrating, but effective.
One of the coolest features of this device is its adjustability.
A small port under your skin connects to the band via a tube.
Through this port, your healthcare provider can add or remove saline, tightening or loosening the band as needed.
The American Journal of Surgery notes that this adjustability allows for a more personalized weight loss journey, which is a major advantage over permanent procedures.
How is a Gastric Band Placed in Your Stomach?
Here are key points on how an adjustable gastric band is placed in the stomach for weight loss:
- Pre-Surgery Preparation: Patients typically undergo medical evaluations and counseling to ensure they are suitable candidates for gastric band surgery.
- Anesthesia: The procedure is performed under general anesthesia, ensuring the patient is unconscious and does not feel pain.
- Laparoscopic Technique: The surgery is minimally invasive, using a laparoscope (a small, tube-like camera) inserted through small incisions in the abdomen.
- Incisions and Access: The surgeon makes 4 to 5 small incisions in the abdomen to insert surgical instruments and the laparoscope for visibility and access.
- Placement of the Band: A silicone adjustable gastric band is wrapped around the upper part of the stomach, creating a small stomach pouch above the band. This limits the amount of food the stomach can hold and slows the passage of food.
- Adjustable Mechanism: The band is connected to a small port placed under the skin of the abdomen. The port allows the surgeon to add or remove saline to tighten or loosen the band, adjusting the level of restriction.
- Adjustments Over Time: After surgery, the band can be tightened or loosened through the port using a needle. This is done based on the patient’s weight loss progress and comfort.
- Shorter Recovery Time: Because the procedure is minimally invasive, recovery time is usually faster than more extensive weight loss surgeries.
- No Permanent Changes to Stomach Anatomy: Unlike procedures that remove parts of the stomach, the adjustable gastric band does not permanently alter the digestive system, and the band can be removed if necessary.
- Monitoring and Follow-Up: Patients require regular follow-up visits to adjust the band, monitor weight loss, and receive nutritional counseling.
Why It is Adjustable: Customizing the Weight Loss Journey
Here is what I realized: No two weight loss journeys are the same.
That is why the adjustable nature of this band is a game-changer. Whether you are losing weight too quickly, too slowly, or experiencing discomfort, your doctor can tweak the band to suit your needs.
This level of customization sets it apart from other weight loss surgeries.
Dr. Linda Parker, a bariatric surgeon, explains, “Patients often need adjustments based on their progress, and having that flexibility is crucial for long-term success.”
So, it is not a one-size-fits-all scenario. It is more like having a tailor for your stomach—a very skilled, medical-grade tailor.
Appetite Suppression: The Science Behind Feeling Full
Let’s talk hormones.
The adjustable gastric band works by altering how your body senses fullness, and hormones like ghrelin play a key role here.
Ghrelin is your hunger hormone, the one whispering sweet nothings about pizza in your ear at midnight.
When the band restricts your stomach size, it also influences ghrelin production, making you feel less hungry.
A study published in Obesity Surgery found that patients who underwent gastric band surgery experienced lower levels of ghrelin, which significantly reduced their appetite.
This hormonal shift is why people feel satisfied with smaller portions.
Think of it as hacking your body’s hunger signals, but with a surgical assist.
Real-Life Example: How Sarah Found Freedom from Food Obsession
Meet Sarah, a 45-year-old mother of two who struggled with obesity her entire adult life.
After trying every diet known to humanity, she opted for a gastric lap band procedure.
“I was skeptical,” she admits. “But after a few adjustments, I noticed I was eating less and actually feeling full.”
Sarah went from eating until she felt physically ill to stopping when she felt satisfied. It was not a miracle; it was science in action, and it changed her life.
Comparing Options: Gastric Band vs. Gastric Sleeve
Now, you might be wondering, “How does a lap band gastric procedure compare to other options like a gastric sleeve?”
Good question.
Both surgeries aim to reduce food intake, but they differ in invasiveness and permanence.
The gastric sleeve involves removing a large part of your stomach, while the adjustable gastric band keeps everything intact.
According to The Journal of Bariatric Surgery, gastric band patients have a shorter recovery time but might lose weight more slowly compared to those who undergo a gastric sleeve operation.
As per LeanAndFit research, “It is a trade-off between flexibility and effectiveness, and your choice will depend on your unique health needs and lifestyle”.
The Psychological Aspect: How Eating Habits Are Transformed?
Weight loss isn’t just about the physical; it is a mental game, too.
Many people who undergo stomach gastric band procedures report a shift in how they view food.
It is no longer about binge-eating for comfort but nourishing the body.
The band serves as a constant reminder to slow down and chew thoroughly—something most of us are guilty of neglecting.
Psychological studies have shown that patients often need counseling to address emotional eating habits.
It is a holistic approach that involves both the mind and the stomach. You also need to learn how to prepare meals that help natural weight loss at home.
FAQs on Adjustable Gastric Bands to Lose Weight
Q-1: How does an adjustable gastric band reduce intake beyond “making the stomach smaller”?
A-1: The band creates a small upper pouch and a narrow, adjustable outlet, which slows the passage of food. That delay increases stretch signals to the brain and encourages earlier meal termination. Because the anatomy isn’t cut or bypassed, digestion remains normal—protein, iron, and B12 absorption are largely preserved compared with malabsorptive procedures. The net effect is portion control and slower eating speed, both of which lower total calories without changing food choices overnight.
Q-2: What makes the band “adjustable,” and when should fills or unfills happen?
A-2: A thin tube connects the band to a subcutaneous port. Clinicians add or remove sterile saline to tighten or loosen the band. Indications for a fill: persistent hunger 1–2 hours after meals, easy tolerance of soft calorie-dense foods, or weight plateau despite adherence. Reasons to unfill: nighttime reflux, frequent regurgitation, painful swallowing, or pregnancy. A good calibration yields “soft stop” fullness with small, protein-forward meals and no reflux.
Q-3: How do bands compare with sleeve or bypass for weight loss and safety?
A-3: Bands typically produce more gradual weight loss than sleeve or bypass but with the advantages of reversibility and no stapling or intestinal rerouting. Early surgical risk is generally lower, and nutritional deficiencies are less common. Trade-offs include the need for ongoing adjustments, device monitoring, and a higher chance of long-term revisions or removal than other procedures. Success hinges on follow-up quality and behavior change rather than the device alone.
Q-4: What day-to-day habits make band results stick—and what are red flags?
A-4: Anchor meals around solid protein first, then vegetables, then modest starch; avoid grazing on soft, high-calorie foods that slip through easily. Take small bites, chew thoroughly, and stop at the first “pressure” cue. Hydrate between meals, not with them. Red flags that warrant a call: sudden reflux, painful swallowing, frequent vomiting, loss of hunger control that appeared after band loosening, or rapid weight regain—any of which can signal maladjustment or band migration.
Q-5: Who tends to do best with a band, and what follow-up should they expect?
A-5: Strong candidates are those seeking a restrictive, reversible option, who are comfortable with regular clinic visits (especially in the first 6–12 months) and ready to follow a structured eating plan. Expect an initial series of adjustments every 4–8 weeks to find the “green zone,” then maintenance visits a few times per year. Programs that pair fills with behavioral coaching, food logging, and step or resistance goals see better long-term weight reduction and fewer complications.
Risks and Considerations: It’s Not All Sunshine and Rainbows
Gastric band surgery may sound like a quick fix for weight loss, but it is far from risk-free. Beneath its minimally invasive reputation lies a list of potential complications that every patient should understand.
Here is a detailed look at the possible risks based on recent clinical findings and patient outcomes.
>>> Band Slippage, Erosion, or Migration:
The band can move out of place, erode into the stomach lining, or migrate entirely. These issues can lead to nausea, vomiting, blockage, or require urgent surgical removal.
>>> Port and Tubing Malfunctions:
The access port used to tighten or loosen the band may flip, leak, or become infected. These problems often necessitate additional procedures, increasing the overall risk.
>>> Gastrointestinal Discomfort:
Patients often experience acid reflux, heartburn, and difficulty swallowing if the band is too tight. Some may feel constant pressure or fullness even after small meals.
>>> Esophageal or Pouch Dilation:
Over time, the area above the band can become overstretched, especially if patients overeat. This can lead to a weakened esophagus and worsened reflux symptoms.
>>> Reoperation and Removal Rates:
Studies indicate that up to 20% of patients eventually need the band removed due to complications or ineffectiveness. In some cases, weight regain follows removal.
>>> Standard Surgical Risks:
Like any surgery, there are risks of infection, internal bleeding, blood clots, and adverse reactions to anesthesia. These risks may be higher for patients with existing health conditions.
>>> Nutritional Deficiencies:
Though gastric banding doesn’t cause malabsorption like some other weight loss surgeries, patients may still develop nutrient deficiencies due to reduced food intake and poor dietary habits.
>>> Inadequate Follow-up Care:
Patients who do not receive regular follow-ups or those who undergo surgery abroad without structured aftercare face a higher likelihood of complications and poor outcomes.
>>> Final Tip:
While gastric band surgery can be an effective tool for weight loss, it is not a guaranteed or effortless solution.
Success depends on proper surgical technique, regular follow-up, lifestyle changes, and close monitoring (such as cognitive restructuring) for complications.
Always consult a qualified bariatric specialist before deciding on this procedure.
Understanding the Role of Adjustable Gastric Bands
Adjustable gastric bands are a fascinating blend of science and surgery, offering a customizable way to tackle obesity.
This medical device, placed around the upper part of the stomach, creates a small pouch that limits food intake, helping individuals feel full faster and consume fewer calories.
Unlike more invasive bariatric surgeries, such as gastric bypass, the adjustable gastric band does not permanently alter the digestive system (just as is the case with bariatric surgery). Instead, it provides a reversible and modifiable approach to weight loss.
One of its key advantages is its adjustability. A surgeon can tighten or loosen the band by injecting or removing saline through a small port placed under the skin, allowing for personalized control over the rate of weight loss.
This adaptability makes it a viable long-term solution for many patients, especially those who need gradual weight reduction.
However, while it is not a magic wand, it can be a life-altering tool for those who commit to the lifestyle changes required. Success with a gastric band depends on adopting healthy eating habits, regular physical activity, and consistent medical follow-ups.
Complications such as band slippage or erosion can occur, but with proper care and monitoring, the adjustable gastric band can be an effective and safe tool in the fight against obesity.
References: