Obesity is much more than just an extra few pounds—it is a complex condition that affects nearly every system in the body.
One of the most concerning consequences of obesity is metabolic dysregulation, a term used to describe the breakdown of normal metabolic processes.
But how does excess weight lead to this imbalance, and why should we be concerned?
In this article, I shall dive deep into the relationship between obesity and metabolic dysregulation, exploring the intricate ways in which these two phenomena are linked.
In This Article:
- Introduction to Obesity and Metabolic Dysregulation
- Understanding Metabolic Dysregulation
- The Role of Fat Cells in Metabolism
- How Obesity Disrupts Insulin Sensitivity
- Inflammation and Metabolic Dysregulation
- FAQs on Metabolic Dysregulation and Obesity
- Hormonal Changes in Obesity
- Daily Lifestyle Habits That Contribute to Metabolic Dysregulation
- Scientific Evidence Connecting Obesity and Metabolic Dysregulation
- Conclusion: How Obesity Leads to Metabolic Dysregulation
Introduction to Obesity and Metabolic Dysregulation
The global obesity epidemic is often discussed in the context of weight loss, diet, and exercise, but the underlying metabolic consequences of obesity are often overlooked.
Metabolic dysregulation refers to the disruption of normal metabolic processes, including how the body processes energy, stores fat, and regulates blood sugar.
When these processes become imbalanced, they can lead to conditions such as type 2 diabetes, cardiovascular disease, and even certain types of cancer.
Obesity is one of the leading causes of metabolic dysregulation, and understanding how it develops is key to tackling this growing health crisis.
Understanding Metabolic Dysregulation
Before we dive into how obesity leads to metabolic dysregulation, it is important to understand what metabolic dysregulation actually means.
In a healthy individual, metabolism functions like a well-oiled machine—nutrients are converted into energy, and hormones like insulin help regulate blood sugar levels.
However, when metabolic dysregulation occurs, this system breaks down.
This breakdown can manifest in various ways, including obesity induced insulin resistance, higher levels of circulating fats (lipids), increased blood sugar, and chronic inflammation.
Over time, these disruptions increase the risk of developing metabolic syndrome, a cluster of conditions that includes high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels.
The Role of Fat Cells in Metabolism
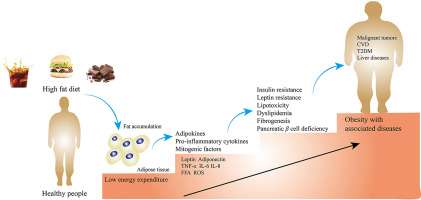
Fat cells, or adipocytes, are more than just storage units for excess energy.
They are metabolically active, secreting hormones and signaling molecules that regulate appetite, insulin sensitivity, and inflammation.
When the body has an excess of fat due to obesity, these fat cells become dysfunctional, and their ability to regulate metabolism is compromised.
This dysfunction is a key driver of metabolic dysregulation.
In an obese individual, the enlarged fat cells secrete harmful substances called adipokines, which promote insulin resistance and chronic inflammation.
This is one reason why obesity is so closely tied to metabolic disorders such as type 2 diabetes.
For instance, when you indulge in a high-fat, high-sugar diet regularly, those extra calories do not just sit there.
Your fat cells are actively releasing chemicals that make it harder for insulin to do its job, contributing to a state of insulin resistance.
This state is a major hallmark of metabolic dysregulation and a precursor to more serious health conditions.
How Obesity Disrupts Insulin Sensitivity?
One of the first signs of metabolic dysregulation is your body’s resistance toward insulin.
Normally, insulin helps your cells absorb glucose (sugar) from the bloodstream to use as energy.
However, in the context of obesity, the body’s cells become less sensitive to insulin, a condition known as insulin resistance.
This happens because excess fat, particularly visceral fat (the type stored around your organs), secretes molecules that interfere with insulin’s ability to signal cells to take up glucose.
As a result, your blood sugar levels rise, leading to high blood sugar—a key component of metabolic dysregulation.
Imagine eating your favorite sugary snack.
In a healthy person, insulin is like a key that opens the door to your cells, allowing sugar to enter and provide energy.
In someone with insulin resistance, the door remains closed, and sugar builds up in the bloodstream, leading to complications like type 2 diabetes.
Inflammation and Metabolic Dysregulation
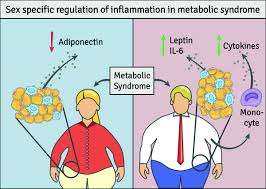
Inflammation is another key player in how obesity leads to metabolic dysregulation. Obesity triggers a state of chronic low-grade inflammation in the body.
This inflammation is driven by the release of inflammatory molecules from enlarged fat cells.
A 2015 study in Nature Reviews Endocrinology demonstrated that the inflammation caused by excess fat disrupts normal metabolic processes and exacerbates insulin resistance.
Over time, this inflammation contributes to a cycle where insulin resistance leads to more fat storage, which in turn leads to more inflammation.
This feedback loop can be difficult to break, especially when poor lifestyle habits, such as a lack of physical activity or a high-calorie diet, continue to fuel the fire.
FAQs on Metabolic Dysregulation and Obesity
Q-1: How does “too much” fat turn into an organ that actively scrambles metabolism?
A-1: As fat cells enlarge, they outgrow their blood supply and become stressed. Stressed adipocytes leak inflammatory signals and free fatty acids (FFAs). Those messengers travel to liver and muscle, jamming insulin signaling and nudging the body to make more glucose and store more fat. Translation: the fat depot stops being a passive pantry and starts acting like a noisy endocrine gland.
Q-2: Why do normal blood sugars sometimes hide serious metabolic trouble?
A-2: The pancreas can overproduce insulin for years to keep glucose in range. Meanwhile, tissues resist that insulin, the liver clears less of it, and fasting insulin creeps up—hyperinsulinemia. You feel “normal,” but the high insulin drives hunger, easier fat storage, and low HDL/high triglycerides. Early tells: large waist, skin tags, and rising triglyceride-to-HDL ratio even with okay glucose.
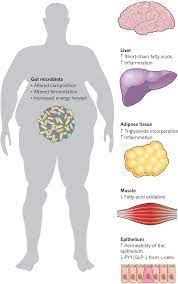
Q-3: What’s the role of “where” fat goes—not just “how much”?
A-3: Visceral and ectopic fat (in liver, muscle, pancreas) are the mischief-makers. Visceral depots drain straight to the liver, bathing it in FFAs and inflammatory cues that boost sugar production and liver fat. As per leanandfit.info research, “Fat in muscle crowds out mitochondria’s work; fat in the pancreas can impair insulin release”. Two people with the same BMI can have very different risk depending on this placement.
Q-4: How do hormones from fat itself tilt the system toward disease?
A-4: Enlarged fat depots shift adipokines: adiponectin (insulin-sensitizing) falls, while leptin rises but the brain becomes less responsive to it. This combo dulls satiety, reduces fat burning, and stiffens blood vessels. Add disrupted daily rhythms—late eating, poor sleep—and you flatten cortisol and melatonin patterns that normally help regulate appetite and glucose control.
Q-5: Can the gut and liver team up to amplify metabolic dysregulation?
A-5: Yes. Lower dietary fiber and altered microbiota can increase gut permeability, letting bacterial fragments enter circulation and stoke inflammation. The liver, already soaked in FFAs from visceral fat, ramps up fat creation and exports triglyceride-rich particles, raising blood lipids. That feedback loop—gut signals + liver fat—pushes toward fatty liver, higher fasting glucose, and hypertension.
What to watch and do: track waist size, morning energy, and triglyceride/HDL ratio alongside glucose; prioritize fiber and protein at meals; shift calories earlier; add daily walking plus 2–3 weekly strength sessions to improve insulin sensitivity; and aim for gradual weight loss—even 5–10% can quiet the inflammatory “noise” and reset metabolic signals.
Hormonal Changes in Obesity
Obesity does not just affect metabolism and inflammation—it also throws hormonal balance out of whack.
Hormones like leptin and ghrelin, which regulate hunger and satiety, become dysregulated in obesity. Leptin is produced by fat cells and signals to your brain when you are full.
However, in obese individuals, the brain becomes resistant to leptin’s signals, leading to overeating despite having sufficient energy stores.
This resistance leads to a vicious cycle where overeating promotes further weight gain, exacerbating metabolic dysregulation.
Additionally, the stress hormone cortisol tends to be higher in people with obesity, further promoting fat storage and metabolic imbalance.
Daily Lifestyle Habits That Contribute to Metabolic Dysregulation
Many everyday lifestyle choices contribute to the development of obesity and, by extension, metabolic dysregulation.
A sedentary lifestyle is one of the biggest contributors.
When you spend hours sitting at a desk, lounging on the couch, or scrolling through social media on your phone, your body is not using energy efficiently.
This leads to fat accumulation, particularly around the abdomen, which we have already discussed as a key player in disrupting metabolism.
Take, for example, a person who regularly consumes fast food, sugary drinks, and processed snacks.
These foods are often high in calories and low in nutrients, contributing to weight gain and increased fat storage.
Over time, this can lead to insulin resistance, inflammation, and hormonal imbalances that drive metabolic dysregulation.
Lack of sleep is another factor. Research shows that insufficient sleep increases hunger hormones, making it harder to control your appetite and leading to overeating.
It is a snowball effect: the more weight you gain, the more likely you are to develop metabolic dysregulation.
Scientific Evidence Connecting Obesity and Metabolic Dysregulation
The link between obesity and metabolic dysregulation is well-documented in scientific literature.
According to a study published in the Journal of Clinical Investigation, obesity-induced insulin resistance is the primary driver of metabolic syndrome.
This study explains that excess fat tissue releases free fatty acids and inflammatory molecules that disrupt insulin signaling, leading to high blood sugar levels and, eventually, type 2 diabetes.
Another study from The Lancet highlights the role of visceral fat in metabolic dysregulation.
It found that individuals with higher levels of abdominal fat were at significantly higher risk for developing insulin resistance and other components of metabolic syndrome, even if their overall body weight was within a healthy range.
These findings underscore the importance of not just weight management but also fat distribution in preventing metabolic disorders. It is not just about how much fat you have, but where it’s located.
How Obesity Leads to Metabolic Dysregulation – My Conclusive Analysis
In conclusion, obesity is a major risk factor for metabolic dysregulation, primarily due to its impact on insulin sensitivity, inflammation, and hormone regulation.
As fat cells grow larger, they release substances that interfere with insulin’s ability to regulate blood sugar, leading to syndrome X—the gateway to metabolic syndrome and other health problems.
Chronic inflammation, driven by excess fat, further exacerbates metabolic dysfunction, while hormonal imbalances create a feedback loop that promotes overeating and further weight gain.
It is a complex, multifaceted problem that affects nearly every system in the body.
If you find yourself living a sedentary lifestyle, consuming a diet rich in processed foods, or experiencing poor sleep patterns, these habits could be contributing to metabolic dysregulation.
While we have explored how obesity leads to metabolic dysfunction, recognizing these patterns can be the first step in preventing further health complications.
References: